Botulism is a rare but fatal disease caused by botulinum toxins released from Clostridium botulinum bacteria. Botulism is categorized into five different forms: foodborne botulism, wound botulism, infant botulism, inhalation botulism, and iatrogenic botulism.
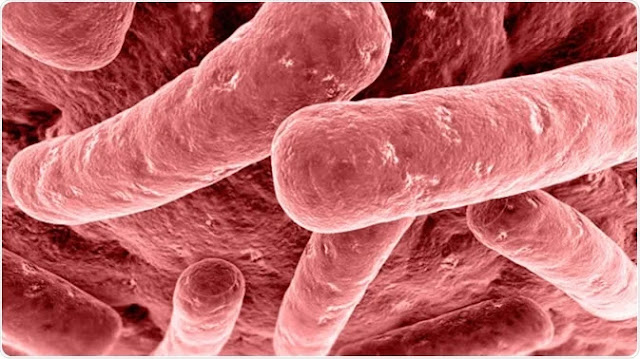 |
| Botulism is a potentially fatal condition that is caused by a bacterium called Clostridium botulinum. |
Agent: Botulinum toxin, produced by the anerobic sporeforming bacterium Clostridium botulinum types A, B, E and rarely F. Type E and F neurotoxins have been recovered from infants with botulism due to C. butyricum and C. barati. C. botulinum is considered a biological warfare agent.
Reservoir: C. botulinum spores are found in soil, dust, honey, marine sediments, and in intestines of fish and land animals.
Transmission: By ingestion of contaminated food (honey in infant botulism), injection of contaminated drugs, or contamination of wounds by soil, dust or gravel. There is no human-to-human transmission.
 |
| Clostridium botulinum gram stain. |
Incubation period: Usually 12–36 hours; sometimes several days; up to 2 weeks for wound botulism. Clinical findings: Descending flaccid skeletal muscle paralysis beginning at the shoulders in the absence of fever; fatigue, weakness, vertigo, blurred vision, dry mouth, difficulty in speaking and swallowing, progressing to an inability to breathe without assistance. Vomiting, diarrhea or constipation may occur. The CFR in the USA after treatment is 5–10%; recovery may take months. Infants present with constipation, anorexia, weakness, an altered cry, difficulty sucking, and swallowing. Muscle weakness progresses in a symmetric descending fashion over hours to a few days. The prognosis is excellent when treated timely.
Diagnostic tests: The diagnosis is initially made from patient’s clinical history and clinical characteristics of the infection. The laboratory confirmation is carried out by analyzing the presence of toxins or bacteria in biological samples, such as stool or blood.
Since the symptoms of botulism are similar to certain diseases (Guillain-Barré syndrome, stroke, myasthenia gravis, and stroke), doctors sometimes perform brain scan, spinal fluid analysis, and nerve/muscle function tests to rule out other diagnoses.
Detection of toxin in serum, stool or wound by mouse inoculation or ELISA; culture of the bacterium from stool or wound; electromyography.
Therapy: The standard of care for treating botulism is administration of antitoxin. It binds directly with the bacterial toxin and prevents it from causing more damage to the nervous system. However, the drug cannot heal the damage already done by the toxins. The mortality rates can be significantly reduced with an immediate antitoxin treatment. In infants, botulism is treated with an antitoxin called botulism immune globulin.
In wound botulism, surgery may be necessary to remove the affected tissue. Antibiotics may be indicated to limit growth of botulism and other co-infecting bacteria in wounds. However, antibiotics are not recommended for other botulism types because these medicines can increase the rate of toxin release.
If the botulism is associated with breathing difficulties, a mechanical ventilator may be used to help the patient breath normally until the severity of symptoms reduces gradually. After completion of the treatment, people who present with fatigue, speech problems, shortness of breath, and swallowing difficulties may need long-term rehabilitation for months or years to recover.
Equine botulinum antitoxin can prevent progression of illness and shorten symptoms in food-borne and wound botulism if administered early. Avoid aminoglycoside antibiotics as these may potentiate the toxin and result in a complete neuromuscular blockade and resultant paralysis.
Prevention: Food for canning or bottling should be thoroughly cooked; consumption of inadequately smoked or salted food and uneviscerated fish should be avoided. Also avoid honey and dusty excavation sites with infants. A pentavalent botulinum toxoid (PBT) vaccine is available from the CDC.
Epidemiology: Rare, but good disease burden data are lacking. Underdiagnosis is common. There are four main types of botulism: intestinal/infant, food-borne, wound and inadvertent. Infant botulism is the most common form of botulism in the USA and is caused by growth of spores germinating the immature gut of infants and releasing the toxin, or rarely in adults with abnormal intestinal tracts. Honey is a common source, but in 85% of infants, the source is unknown. Infant cases occur from 6 days to 12 months of age and affect equally both sexes. Food-borne botulism is the result of eating fermented, salted, or smoked fish, seafood or meat that has not been cured for long enough to eliminate contamination. It is also due to incorrect home canning or bottling of vegetables or fruit. Botulism usually occurs in outbreaks in those exposed to the same food. The largest numer of reported cases per country over the decade 2000–2009 in ProMED mail have occurred in Thailand (83 cases from deer meat, 163 from bamboo shoots), Poland (276 from preserved food), and Georgia (217 from home-preserved – vegetables). Food-borne botulism outbreaks occur in indigenous tribes in Alaska and Canada by consuming improperly preserved fish products (seal, salmon, salmon eggs). Wound botulism results from failure to remove contaminated soil completely from wounds and sealing them, permitting anaerobic growth of the bacteria. Inadvertent botulism is a recent phenomenon resulting from the use of diluted Botulinum toxin to treat patients for several disorders and for cosmetic reasons.
References
No comments:
Post a Comment