Left superior vena cava (LSVC) is the most common congenital malformation of the thoracic venous return and is present in 0.3 to 0.5% of individuals in the general population with a normal heart, and 4.5% in individuals with congenital heart diseases. A LSVC co-occurs with the right superior vena cava in 80 to 90% of cases, 2 and may also be accompanied by other heart abnormalities, such as anomalous connections of the pulmonary veins, aortic coarctation, tetralogy of Fallot, transposition of the great vessels as well as dextroversion. Moreover, cardiac rhythm disturbances concerning impulse formation and conduction have been observed.
 |
| Left superior vena cava |
The LSVC
usually drains into the right atrium (in 80–92%) through a dilated coronary
sinus (CS),5,6 but in approximately 10 to 20% of cases, it is associated with
left atrial (LA) drainage. The LSVC may drain directly through the left atrium
or via the unroofed CS, which is a cause of right-to-left cardiac shunt. The
majority of patients with LSVC are asymptomatic. In general, only patients with
unusual drainage and right-to-left shunting are of clinical significance.
Anomalous venous return via the LSVC may be the cause of cardiac arrhythmias,
decreased exercise tolerance, progressive fatigue, chest discomfort,
palpitations, syncope or cyanosis.
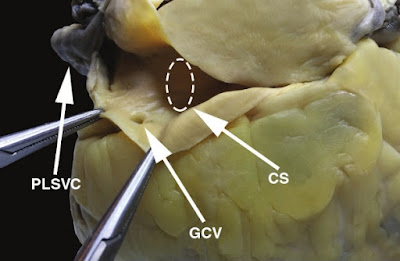 |
| The left superior vena cava drains into the coronary sinus in this heart specimen. CS, coronary sinus; GCV, great cardiac vein; PLSVC, persistent left superior vena cava. |
The implications of existing LSVC could be important for clinicians who are involved in placement of central venous-access devices.
📖 Netter’s Cardiology 2th Edition
Access to the right
side of the heart or pulmonary vasculature through the left subclavian vein is
much more difficult in patients with LSVC. Placement of a central line or
cardiac resynchronisation therapy leads and pacemaker implantation in
undiagnosed cases with LSVC can result in incorrect positioning. In those
cases, access to the right heart and coronary sinus should be performed via the
right subclavian vein, allowing for an easier route. Also the presence of LSVC
is a relative contraindication to the administration of retrograde cardioplegia
during cardiac surgery.
 |
| View of the internal surface of the right atrium. CSO, coronary sinus ostium; EuchV, Eustachian valve; IVC, inferior vena cava. |
The right LSVC
is usually present as well but may be absent. The two venae cavae may be equal
in size, or one (generally the left) may be smaller than its counterpart. The
left innominate vein, if present, is smaller than normal or may be more or less
plexiform.
The coronary sinus ostium (coronary os) is very large because of the increased blood flow through it, detected easily by cardiac ultrasound. Occasionally, a defect is present in the wall between the sinus and left atrium (unroofed coronary sinus). Generally, such a defect results in a left-to-right shunt; that is, left atrial blood enters the coronary sinus and is carried to the right atrium. Hemodynamically, therefore, the anomaly resembles an atrial septal defect. If the defect is extremely large, particularly if the coronary os is small or atretic, the left SVC is said to “enter the left atrium.”
Depending
on the timing of the scan and the side of the injection variable amounts of
contrast may be seen within the vessel.
CT is also
able, especially with the benefit of reformats, to delineate the site of
drainage (usually coronary sinus).
References
1. Zhong YL, Long X-M, Jiang L-Y, He B-F, Lin H, Luo P. et al. Surgical treatment of dextroversion, isolated persistent left superior vena cava draining into the left atrium. J Card Surg. 2015;30(10):767–770. [PubMed] [Google Scholar]
2. Ruano, CA, Marinho-da-Silva A, Donato P. Congenital thoracic venous anomalies in adults: morphologic MR imaging. Curr Probl Diagn Radiol. 2015;44(4):337–345. [PubMed] [Google Scholar]
3. Kula S, Cevik A, Sanli C, Pektas A, Tunaoglu FS, Oguz AD. et al. Persistent left superior vena cava: experience of a tertiary health-care center. Pediatr Int. 2011;53(6):1066–1069. [PubMed] [Google Scholar]
4. Buirski G, Jordan SC, Joffe HS, Wilde P. Superior vena caval abnormalities: their occurrence rate, associated cardiac abnormalities and angiographic classification in a paediatric population with congenital heart disease. Clin Radiol. 1986;37(2):131–138. [PubMed] [Google Scholar]
5. Granata A, Andrulli S, Fiorini F, Logias F, Figuera M, Mignani R. et al. Persistent left superior vena cava: what the interventional nephrologist needs to know. J Vasc Access. 2009;10(3):207–211. [PubMed] [Google Scholar]
6. Goyal SK, Punnam SR, Verma G, Ruberg FL. Persistent left superior vena cava: a case report and review of literature. Cardiovasc Ultrasound. 2008;6:50–50. [PMC free article] [PubMed] [Google Scholar]
7. Dinasarapu CR, Adiga GU, Malik S. Recurrent cerebral embolism associated with indwelling catheter in the presence of anomalous neck venous structures. Am J Med Sci. 2010;340(5):421–423. [PubMed] [Google Scholar]
8. Uçar O, Paşaoğlu L, Ciçekçioğlu H, Vural M, Kocaoğlu I, Aydoğdu S. Persistent left superior vena cava with absent right superior vena cava: a case report and review of the literature. Cardiovasc J Afr. 2010;21(3):164–166. [PMC free article] [PubMed] [Google Scholar]
9. Povoski SP. A prospective analysis of the cephalic vein cutdown approach for chronic indwelling central venous access in 100 consecutive cancer patients. Ann Surg Oncol. 2000;7(7):496–502. [PubMed] [Google Scholar]
10. Lai YC, Goh JC, Lim SH, Seah TG. Difficult pulmonary artery catheterization in a patient with persistent left superior vena cava. Anaesth Intensive Care. 1998;26(6):671–673. [PubMed] [Google Scholar]
11. Hołda M, Koziej M, Hołda J, Piątek K, Tyrak K, Chołopiak W. et al. Atrial septal pouch – morphological features and clinical considerations. int J Cardiol. 2016;220:337–342. [PubMed] [Google Scholar]
12. Pasquini L, Belmar C, Seale A, Gardiner HM. Prenatal diagnosis of absent right and persistent left superior vena cava. Prenat Diagn. 2006;26(8):700–702. [PubMed] [Google Scholar]
13. Miraldi F, di Gioiga CR, Proietti P, De Santis M, d'Amati G, Gallo P. Cardinal vein isomerism: an embryological hypothesis to explain a persistent left superior vena cava draining into the roof of the left atrium in the absence of coronary sinus and atrial septal defect. Cardiovasc Pathol. 2002;11(3):149–152. [PubMed] [Google Scholar]
14. Hołda MK, Klimek-Piotrowska W, Koziej M, Mazur M. Anatomical variations of the coronary sinus valve (Thebesian valve): implications for electrocardiological procedures. Europace. 2015;17(6):921–927. [PubMed] [Google Scholar]
15. Klimek-Piotrowska W, Hołda MK, Koziej M, Piątek K, Hołda J. Anatomy of the true interatrial septum for transseptal access to the left atrium. Ann Anat, Anatomischer Anzeiger. 2016;205:60–64. [PubMed] [Google Scholar]
16. Klimek-Piiotrowska W, Hołda MK, Piątek K, Koziej M, Hołda J. Normal distal pulmonary vein anatomy. Peer J. 2016;4:e1579–e1579. [PMC free article] [PubMed] [Google Scholar]
17. Povoski SP. Persistent left superior vena cava: review of the literature, clinical implications, and relevance of alterations in thoracic central venous anatomy as pertaining to the general principles of central venous access device placement and venography in cancer patients. World J Surg Oncol. 2011;9:173–173. [PMC free article] [PubMed] [Google Scholar]
18. Lenox CC, Zuberbuhler JR, Park SC, Neches WH, Mathews RA, Fricker FJ. et al. Absent right superior vena cava with persistent left superior vena cava: implications and management. Am J Cardiol. 1980;45(1):117–122. [PubMed] [Google Scholar]
19. Lee MS, Pande RL, Rao B, Landzberg MJ, Kwong RY. Cerebral abscess due to persistent left superior vena cava draining into the left atrium. Circulation. 2011;124(21):2362–2364. [PubMed] [Google Scholar]
20. Sarodia BD, Stoller JK. Persistent left superior vena cava: case report and literature review. Respir Care. 2000;45(4):411–416. [PubMed] [Google Scholar]
21. Elison B, Evans D, Zanders T, Jeanmonod R. Persistent left superior vena cava draining into the pulmonary venous system discovered after central venous catheter placement. Am J Emerg Med. 2014;32(8):943.e1–3. [PubMed] [Google Scholar]
22. Erdoğan M, Karakaş P, Uygur F, Meşe B, Yamak B, Bozkir MG. Persistent left superior vena cava: the anatomical and surgical importance. West Indian Med J. 2007;56(1):72–76. [PubMed] [Google Scholar]
23. Heye T, Wengenroth M, Schipp A, Dengler JT, Grenacher L, Kauffmann WG. Persistent left superior vena cava with absent right superior vena cava: morphological CT features and clinical implications. Int J Cardiol. 2007;116(3):e103–105. [PubMed] [Google Scholar]
24. luckianow G, Cole D, Kaplan L. Anatomical variant found during catheter insertion. J Am Acad Phys Assist. 2009;22(9):60–63. [PubMed] [Google Scholar]
25. Liu X, He Y, Tian Z, Rychik J. Persistent left superior vena cava connected to the coronary sinus in the fetus: effects on cardiac structure and flow dynamics. Pediatr Cardiol. 2016;37(6):1085–1090. [PubMed] [Google Scholar]
Tags: left superior vena cava to coronary sinus, left superior vena cava baby, left superior vena cava radiology, left superior vena cava draining to the coronary sinus, left superior vena cava syndrome, left superior vena cava in fetus, left superior vena cava radiopaedia, left superior vena cava to left atrium, left superior vena cava anomalous venous drainage, left superior vena cava anomaly, left superior vena cava artery, persistent left superior vena cava associated anomalies, persistent left superior vena cava anatomy, persistent left superior vena cava arrhythmia, persistent left superior vena cava and pacemaker, persistent left superior vena cava atrial fibrillation, a persistent left superior vena cava, ligament of left superior vena cava, is there a left superior vena cava, significance of left superior vena cava
No comments:
Post a Comment