The protective response of vomiting is an example of central regulation of gut motility functions. Vomiting starts with salivation and the sensation of nausea. Reverse peristalsis empties material from the upper part of the small intestine into the stomach. The glottis closes, preventing aspiration of vomitus into the trachea. The breath is held in mid inspiration. The muscles of the abdominal wall contract, and because the chest is held in a fixed position, the contraction increases intra-abdominal pressure. The LES and the esophagus relax, and the gastric contents are ejected. The “vomiting center” in the reticular formation of the medulla consists of various scattered groups of neurons in this region that control the different components of the vomiting act.
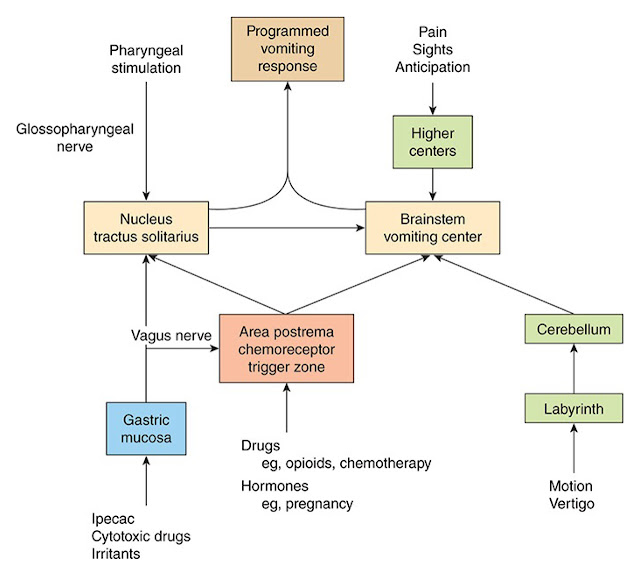 |
| Neural pathways leading to the initiation of vomiting in response to various stimuli. |
Irritation of the mucosa of the upper gastrointestinal tract is one trigger for vomiting. Impulses are relayed from the mucosa to the medulla over visceral afferent pathways in the sympathetic nerves and vagi. Other causes of vomiting can arise centrally. For example, afferents from the vestibular nuclei mediate the nausea and vomiting of motion sickness. Other afferents presumably reach the vomiting control areas from the diencephalon and limbic system, because emetic responses to emotionally charged stimuli also occur.