(Baastrup’s disease, Kissing spines syndrome)
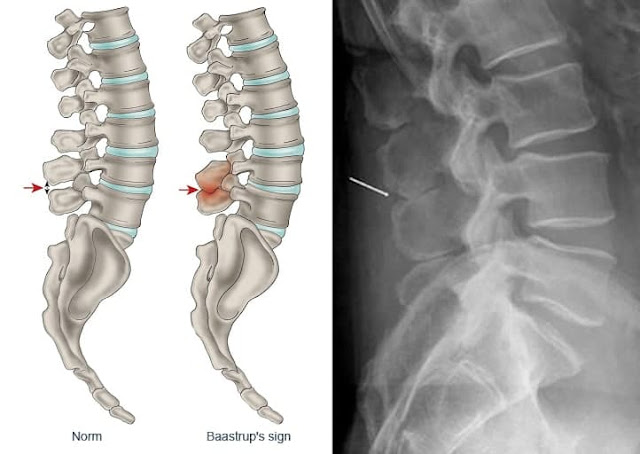
Excessive lordosis is a common finding and may produce mechanical pressure that causes repetitive strains of the interspinous ligament with subsequent degeneration and collapse. Baastrup’s disease (kissing spine syndrome) is a term referring to close approximation of adjacent spinous processes due to degenerative changes of the spine.
 |
| Baastrup’s disease |
Baastrup’s disease usually affects the lumbar spine, with L4-L5 being the most commonly affected level. There is higher occurrence at ages over 70 and no gender predilection. Symptoms include back pain with midline distribution that worsens during extension, is relieved during flexion and is exaggerated upon finger pressure at the level of interest. Diagnosis rests on clinical examination and imaging studies. The hallmark of imaging findings is the close approximation and contact of adjacent spinous processes, with all the subsequent findings including oedema, cystic lesions, sclerosis, flattening and enlargement of the articulating surfaces, bursitis and occasionally epidural cysts or midline epidural fibrotic masses. Proposed therapies include conservative treatment, percutaneous infiltrations or surgical therapies such as excision of the bursa or osteotomy.
Pathogenesis
Baastrup’s disease is a term referring to close approximation of adjacent spinous processes due to general degenerative changes of the spine. Usually there is an excessive lordosis with resultant mechanical pressure process that causes repetitive strains of the interspinous ligament with subsequent degeneration and collapse.
📖 Practical Office Orthopedics
Thus, adjacent spinous processes come in contact and during repetitive shearing movements there is further inflammation of an adventitious bursa present in the interspinous space. Furthermore, these repetitive shearing movements of the closely approximated spinous processes result in additional architectural distortion, flattening, sclerosis and cyst formation in the opposing surfaces. Changes in Baastrup’s disease in most cases occur in association with other degenerative factors such as loss of disc height, spondylolisthesis and spondylosis with osteophyte formation. However, in the literature there are reports in the literature of patients independently developing Baastrup’s disease in the absence of the aforementioned factors.
Baastrup’s disease usually affects the lumbar spine with L4-L5 being the most commonly affected level. In most of the cases, only one level is affected and further degenerative changes (such as facet joints hypertrophy, intervertebral disc herniation or spondylolisthesis) can be seen in this pathological leve. Concerning the frequency of Baastrup’s disease, studies show a decade-on-decade increase with higher occurrence at ages over 70 and no gender predilection.
In standard lateral X-rays of the spine the most common finding is the close approximation and contact of adjacent spinous processes with sclerosis of the articulating surfaces. Additionally, in more severe cases there is flattening and enlargement of the articulating surfaces or articulation of the two affected spinous processes. Furthermore, general degenerative changes in the spine can be seen, usually most prominent at the pathological level. Advantages of radiographic imaging include the low cost and wide availability of the technique and a relatively low ionising radiation dose. On the other hand, there is poor imaging quality especially at the lower lumbar levels of obese patients.
Treatment
Proposed therapies include conservative course of analgesics and non-steroid anti-inflammatory drugs, percutaneous infiltrations with long acting corticosteroids mixed to local anaesthetic or surgical therapies such as excision of the bursa or osteotomy. Specifically for the percutaneous infiltrations, imaging guidance ensures accurate needle positioning with resultant increase of technical and clinical efficacy and at the same time decrease of potential complications rate. Surgery with either partial or total excision of the spinous processes does not always result in pain alleviation. The moderate efficacy of surgical approaches led certain investigators to the theory that kissing spine syndrome is not an actual disease but rather a part of degenerative spinal changes, mainly spondylosis with osteophyte formation. More recent studies suggest that Baastrup’s sign should raise the suspicion of a bursitis.
In certain degenerative disorders of the spine, the initial pain reductive effect of conservative therapy does not last and there are relapses in long term follow-up since the causative factor(s) has not been treated. Diagnosis of Baastrup’s disease is important in case of minimally invasive imaging-guided or surgical therapies. In case of misdiagnosis (e.g. facet joint syndrome or intervertebral disc pathology) one will respectively perform intra-articular or epidural infiltration rather than injection at the level of interspinous ligament.
Christian Ingerslev Baastrup (1855 - 1950), Danish radiologist.
 |
| Christian Ingerslev Baastrup |
Christian Ingerslev Baastrup was the son of the wine merchant Carl Lauritz Baastrup and Christiane Margrethe from Ingerslev. He attended Borgerdydskolen in Copenhagen and graduated in medicine from the University of Copenhagen in 1909. After serving his internship in various hospitals, and working as assistant physician in departments of otolaryngology and ophthalmology, he was assistant in the radiological clinic at Rigshospitalet 1911-1913. From 1912 he was a radiologist at the clinic of professor Lorentzen. He subsequently worked at the roentgenological clinics of the Kommunehospitalet and Bispebjerg hospital, where he was chief of the X-ray clinic from 1922 and was appointed physician-in-chief in 1935.
Baastrup participated in a large number of international radiological conventions and was a collaborator in the journal Acta radiologica. He was c-founder of Nordisk Forening for Radiologi (Oslo) in 1919, and initiated the establishment of a museum of medical history, for which he secured one of the world's largest and most complete collections of X ray apparatuses. He was a member of the Deutsche Röntgengesellschaft and Membre titulaire Société de Radiologie médicale de France.
References
1. Kelekis A, Filippiadis DK, Martin JB, Brountzos E. Standards of practice: quality assurance guidelines for percutaneous treatments of intervertebral discs. Cardiovasc Intervent Radiol. 2010;33(5):909–913. doi: 10.1007/s00270-010-9952-5. [PubMed] [CrossRef] [Google Scholar]
2. Data S, Lee M, Falco F, Bryce D, Hayek S. Systematic assessment of diagnostic accuracy and therapeutic utility of lumbar facet joint interventions. Pain Physician. 2009;12:437–460. [PubMed] [Google Scholar]
3. Abdi S, Datta S, Trescot AM, Schultz DM, Adlaka R, Atluri SL, Smith HS, Manchikanti L. Epidural steroids in the management of chronic spinal pain: a systematic review. Pain Physician. 2007;10:185–212. [PubMed] [Google Scholar]
4. Barz T, Melloh M, Lord SJ, Kasch R, Merk HR, Staub LP. A conceptual model of compensation/decompensation in lumbar segmental instability. Med Hypotheses. 2014;83(3):312–316. doi: 10.1016/j.mehy.2014.06.003. [PubMed] [CrossRef] [Google Scholar]
5. Kelekis A, Filippiadis D. Percutaneous therapy versus surgery in chronic back pain: how important is imaging in decision-making? Imaging Med. 2013;5(2):187–196. doi: 10.2217/iim.13.15. [CrossRef] [Google Scholar]
6. Baastrup C. On the spinous processes of the lumbar vertebrae and the soft tissues between them, and on pathological changes in that region. Acta Radiol. 1933;14:52–54. doi: 10.3109/00016923309132353. [CrossRef] [Google Scholar]
7. Brailsford J. Deformities of the lumbo-sacral regions of the spine. Br J Surg. 1929;16:562–627. doi: 10.1002/bjs.1800166405. [CrossRef] [Google Scholar]
8. Kwong Y, Rao N, Latief K. MDCT findings in Baastrup disease: disease of normal feature of the aging spine. AJR Am J Roentgenol. 2011;196:1156–1159. doi: 10.2214/AJR.10.5719. [PubMed] [CrossRef] [Google Scholar]
9. Lamer TJ, Tiede JM, Fenton DS. Fluoroscopically-guided injections to treat “kissing spine” disease. Pain Physician. 2008;11:549–554. [PubMed] [Google Scholar]
10. Singla A, Shankar V, Mittal S, Agarwal A, Garg B. Baastrup’s disease: the kissing spine. World J Clin Cases. 2014;2(2):45–47. doi: 10.12998/wjcc.v2.i2.45. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Maes R, Morrison WB, Parker L, Schweitzer ME, Carrino JA. Lumbar interspinous bursitis (Baastrup disease) in a symptomatic population: prevalence on magnetic resonance imaging. Spine (Phila Pa 1976) 2008;33(7):E211–E215. doi: 10.1097/BRS.0b013e318169614a. [PubMed] [CrossRef] [Google Scholar]
12. Bywaters EG, Evans S. The lumbar interspinous bursae and Baastrup’s syndrome an autopsy study. Rheumatol Int. 1982;2:87–96. doi: 10.1007/BF00541251. [PubMed] [CrossRef] [Google Scholar]
13. Beks JW. Kissing spines: fact or fancy? Acta Neurochir (Wein) 1989;100:134–135. doi: 10.1007/BF01403600. [PubMed] [CrossRef] [Google Scholar]
14. DePalma MJ, Slipman CW, Siegelman E, et al. Interspinous bursitis in an athlete. J Bone Joint Surg (Br) 2004;86:1062–1064. doi: 10.1302/0301-620X.86B7.15154. [PubMed] [CrossRef] [Google Scholar]
15. Jang EC, Song KS, Lee HJ, Kim JY, Yang JJ. Posterior epidural fibrotic mass associated with Baastrup’s disease. Eur Spine J. 2010;19(Suppl 2):S165–S168. doi: 10.1007/s00586-009-1262-8. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
16. Chen CK, Yeh L, Resnick D, Lai PH, Liang HL, Pan HB, Yang CF. Intraspinal posterior epidural cysts associated with Baastrup’s disease: report of 10 patients. AJR Am J Roentgenol. 2004;182:191–194. doi: 10.2214/ajr.182.1.1820191. [PubMed] [CrossRef] [Google Scholar]
17. Woo CC. Hyperostosis of lumbar spinous process: a radiological feature in a young acromegalic. J Manip Physiol Ther. 1987;10(3):111–115. [PubMed] [Google Scholar]
18. Arias Fernández J, Broncano Cabrero J, Bondía Gracia JM, Aquerreta Beola JD. Radiological manifestations of Baastrup’s disease in children. Radiol. 2013;55(5):447–450. [PubMed] [Google Scholar]
19. Hui C, Cox I. Two unusual presentations of Baastrup disease. Clin Radiol. 2007;62:495–497. doi: 10.1016/j.crad.2006.12.003. [PubMed] [CrossRef] [Google Scholar]
20. Santiago FR, Kelekis A, Alvarez LG, Filippiadis DK. Interventional procedures of the spine. Semin Musculoskelet Radiol. 2014;18(3):309–317. doi: 10.1055/s-0034-1375572. [PubMed] [CrossRef] [Google Scholar]
21. Erginousakis D, Filippiadis DK, Malagari A, Kostakos A, Brountzos E, Kelekis NL, Kelekis A. Comparative prospective randomized study comparing conservative treatment and percutaneous disk decompression for treatment of intervertebral disk herniation. Radiology. 2011;260(2):487–493. doi: 10.1148/radiol.
baastrup sign radiopaedia, baastrup significado, que significa baastrup, baastrup’s syndrome, baastrup's syndrome, baastrup's, baastrup's phenomenon, o que significa baastrup

No comments:
Post a Comment