Dagnini’s reflex ( Aschner-Dagnini test, Oculocardiac Reflex)
 |
| Dagnini’s reflex ( Aschner-Dagnini test, Oculocardiac Reflex ) |
The oculocardiac reflex (OCR), also known as the Aschner reflex or trigeminovagal reflex (TVR), was first described in 1908 as a reduction in heart rate secondary to direct pressure placed on the eyeball. It is defined by a decrease in heart rate by greater than 20% following globe pressure or traction of the extraocular muscles. The reflex most commonly results in sinus bradycardia. However, it also has a reported association with reduced arterial pressure, arrhythmia, asystole, and even cardiac arrest. This reflex has most notably been depicted during ophthalmologic procedures, more specifically during strabismus surgery; however, it also may be activated by facial trauma, regional anesthetic nerve blocks, and mechanical stimulation. This activity describes the oculocardiac reflex and highlights the role of the interprofessional team in the management of patients with the symptoms during surgery.
Anatomy and Physiology
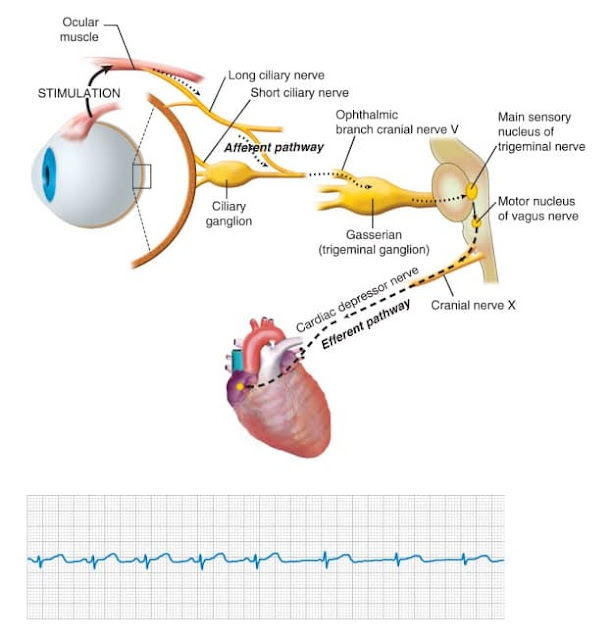
The OCR arc consists of an afferent and efferent limb. The trigeminal nerve, otherwise known as the fifth cranial nerve, serves as the sensory afferent limb.
📖 Hurst’s the Heart, 14th Edition: Two Volume Set
The vagus nerve, also known as cranial nerve ten, comprises the efferent limb of the OCR. The pathway is initiated by the activation of stretch receptors in the ocular and periorbital tissues. The short and long ciliary nerves conduct impulses that carry the sensory message to the ciliary ganglion. From there the impulses are transported by way of the ophthalmic division of the trigeminal nerve to the Gasserian ganglion, followed by the trigeminal nucleus, where the afferent limb will terminate in the central nervous system (CNS). The CNS will then process this sensory information, and internuclear communication will occur between the trigeminal sensory nucleus and the visceral motor nucleus of the vagus nerve. This stimulates the efferent limb, causing impulses to exit the brainstem and transmit to the myocardium to synapse as the sinoatrial node and activate the vagal motor response. The resultant effects include negative chronotropy, leading to bradycardia.
Risk Factors
The OCR has been associated with various triggering stimuli, with the most common being traction to the extraocular muscles. Multiple studies have reported an increased incidence with medial rectus traction when compared to other ocular muscles. However, there also have been studies reporting no increased association with traction to a specific extraocular muscle over another.
Additional stimuli that have been linked to triggering the OCR include direct pressure to the globe, ocular manipulation, and ocular pain. Secondary to increased pressure, retrobulbar blocks, ocular hematomas, and facial or orbital trauma also may induce activation of the reflex. It is also important to note that this is a fatigable reflex, meaning its intensity will decrease with multiple, repeated stimuli.
Clinical Significance
Though the most common side effect of the OCR is bradycardia, one must worry about a further decline to potentially fatal arrhythmias, asystole, and even cardiac arrest. In two studies, one in 1973 by Apt et al. and another in 2015 by Espahbodi et al. reported the OCR occurrence rate of OCR in patients undergoing ophthalmologic surgeries as 67.9% and 63% respectively. Though the majority of these patients do not experience detrimental outcomes following activation of the OCR, the potential makes this phenomenon important to note.
Activation of the OCR also has been associated with noncardiac consequences. Due to the activation of the vagal motor response, other vagal effects reported include hypotensive episodes, syncope, and gastrointestinal responses such as nausea and vomiting. This has been questioned to have an impact on the severity of postoperative nausea and vomiting (PONV). In the pediatric population, the incidence of PONV has been reported to be as high as 85% following strabismus surgery and is the most common reason for inpatient admission following an outpatient procedure.
When discussing the prevention and treatment of the OCR and its potentially devastating consequences, it is important to know that the only definitive treatment is the immediate cessation of the triggering stimulus. When in the operating room, immediate removal of pressure to the globe of the eye or surrounding orbital tissues can terminate the reflex. The next step of the procedure is to proceed with caution. Unfortunately, in less controlled circumstances, such as trauma, cessation of the triggering stimulus can be more challenging. In these instances, pharmacologic management may be required, and cardiac monitoring should be initiated.
Additionally, it is important to know what anesthetic agents can be used to help decrease OCR occurrence, as the incidence may vary with each agent used. Multiple studies have shown that pretreatment with intravenous anticholinergics, such as atropine or glycopyrrolate, decreases the incidence of OCR. Atropine works by blocking peripheral muscarinic receptors of the heart and causes increased firing at the sinoatrial node as well as conduction through the AV node. This opposes the vagal response, or the efferent limb, of the OCR. Through its stimulation of sympathetic activity, ketamine may counteract vagal stimulation caused by OCR. A study by Choi et al. reported a lower incidence of OCR when a ketamine infusion was used as the primary anesthetic agent when compared to sevoflurane, halothane, and propofol. Ketamine was reported by Espahbodi et al. in 2015 to be superior to atropine in decreasing the incidence of OCR. In another study, ketamine also was associated with a lower incidence of postoperative nausea, vomiting, and agitation.
Blunting the afferent limb of the reflex arc can also decrease OCR occurrence. This can be done using a retro or peribulbar block with xylocaine hydrochloride to block the ciliary ganglion. This in combination with another agent shown to decreased OCR incidence, such as atropine, can provide further protection from OCR activation.
It is important to note that the administration of fast-acting opioids, such as fentanyl, sufentanil, and remifentanil, can potentially facilitate bradycardia caused by the OCR. Many anesthetic agents have been studied regarding their effects on OCR, and it is crucial to know how each acts on the reflex. Many still require further investigation. However, it has repeatedly been reported that pr-anesthetic medication with atropine, retrobulbar blocks, or other agents used to blunt the OCR should be routinely utilized during procedures or traumas related to the eye. This is to protect patients against the potential consequences of OCR activation.
References- 1.
- Waldschmidt B, Gordon N. Anesthesia for pediatric ophthalmologic surgery. J AAPOS. 2019 Jun;23(3):127-131. [PubMed]
- 2.
- Dunphy L, Anand P. Paediatric orbital trapdoor fracture misdiagnosed as a head injury: a cautionary tale! BMJ Case Rep. 2019 Apr 03;12(4) [PMC free article] [PubMed]
- 3.
- Arnold RW, Bond AN, McCall M, Lunoe L. The oculocardiac reflex and depth of anesthesia measured by brain wave. BMC Anesthesiol. 2019 Mar 14;19(1):36. [PMC free article] [PubMed]
- 4.
- Rahimi Varposhti M, Moradi Farsani D, Ghadimi K, Asadi M. Reduction of oculocardiac reflex with Tetracaine eye drop in strabismus surgery. Strabismus. 2019 Mar;27(1):1-5. [PubMed]
- 5.
- Jean YK, Kam D, Gayer S, Palte HD, Stein ALS. Regional Anesthesia for Pediatric Ophthalmic Surgery: A Review of the Literature. Anesth Analg. 2020 May;130(5):1351-1363. [PubMed]
- 6.
- Shakil H, Wang AP, Horth DA, Nair SS, Reddy KKV. Trigeminocardiac Reflex: Case Report and Literature Review of Intraoperative Asystole in Response to Manipulation of the Temporalis Muscle. World Neurosurg. 2019 Feb;122:424-427. [PubMed]
- 7.
- Ducloyer JB, Couret C, Magne C, Lejus-Bourdeau C, Weber M, Le Meur G, Lebranchu P. Prospective evaluation of anesthetic protocols during pediatric ophthalmic surgery. Eur J Ophthalmol. 2019 Nov;29(6):606-614. [PubMed]
- 8.
- Başağaoğlu B, Steinberg A, Tung IT, Olorunnipa S, Maricevich RS. Oculocardiac Reflex as a Late Presentation of Orbital Floor Fracture. J Craniofac Surg. 2018 Oct;29(7):e720-e722. [PubMed]
- 9.
- Bloch M. Oculocardiac reflex: 'My heart just stopped'. Emerg Med Australas. 2018 Aug;30(4):592-593. [PubMed]
- 10.
- Arnold RW, Biggs RE, Beerle BJ. Intravenous dexmedetomidine augments the oculocardiac reflex. J AAPOS. 2018 Jun;22(3):211-213.e1. [PubMed]
- 11.
- DesPain AW, Chapman J, Shaukat H. Oculocardiac Reflex in a Pediatric Trauma Patient. Pediatr Emerg Care. 2020 Jul;36(7):e399-e401. [PubMed]
dagnini reflex, dagnini aschner reflex, what is startling reflex, aschner dagnini reflex
No comments:
Post a Comment