Calciphylaxis (calcific uremic arteriolopathy) results from deposition of calcium in the tunica media portion of the small vessel walls in association with proliferation of the intimal layer of endothelial cells.
 |
It is almost always associated with end-stage renal disease, especially in patients undergoing chronic dialysis (either peritoneal dialysis or hemodialysis). It has been reported to occur in up to 5% of patients who have been on dialysis for longer than 1 year. Calciphylaxis typically manifests as nonhealing skin ulcers located in adiposerich areas of the trunk and thighs, but the lesions can occur anywhere. They are believed to be caused by an abnormal ratio of calcium and phosphorus, which leads to the abnormal deposition within the tunica media of small blood vessels. This eventually results in thrombosis and ulceration of the overlying skin. Calciphylaxis has a poor prognosis, and there are few well-studied therapies.
Clinical Findings: Calciphylaxis is almost exclusively seen in patients with chronic end-stage renal disease. Most patients have been on one form of dialysis for at least 1 year by the time of presentation.
 |
| Calciphylaxis |
The initial presenting sign is that of a tender, dusky red to purple macule that quickly ulcerates. The ulcerations have a ragged border and a thick black necrotic eschar. The ulcers tend to increase in size, and new areas appear before older ulcers have any opportunity to heal.
📖 Critical Care Nephrology 3rd Edition
Ulcerations begin proximally and tend to follow the path of the underlying affected blood vessel. Their most prominent location is within the adipose-rich areas of the trunk and thighs, especially the abdomen and mammary regions. Patients often report that ulcerations form in areas of trauma. The main differential diagnosis is between an infectious cause and calciphylaxis. Skin biopsies and cultures can be performed to differentiate the two. Skin biopsies are diagnostic. Radiographs of the region often show calcification of the small vessels, and this can be used to support the diagnosis. Patients who develop calciphylaxis have a poor prognosis, with the mortality rate reaching 80% in some series. For some unknown reason, those with truncal disease tend to survive longer than those with distal extremity disease. Complications caused by the chronic severe ulcerations (e.g., infection, sepsis) are the main cause of mortality.
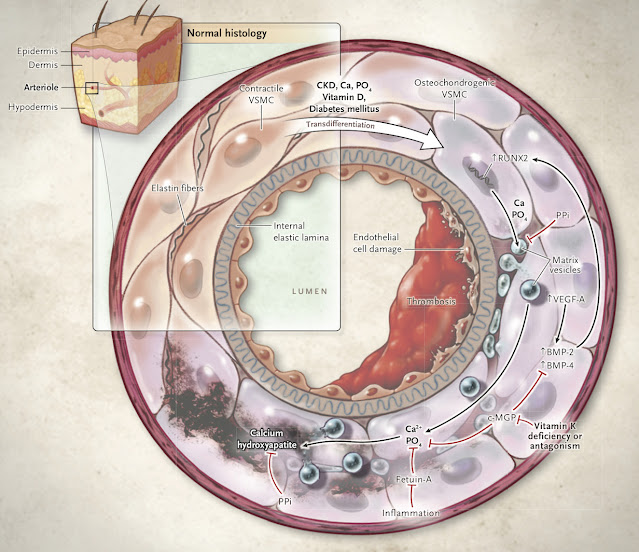 |
| Pathogenesis of Calciphylaxis |
Pathogenesis: The exact mechanism of calcification of the tunica media of blood vessels in calciphylaxis is not completely understood. The fact that it is seen almost exclusively in patients undergoing chronic dialysis therapy has led to many theories on its origin. The final mechanism is a hardening of the vessel wall with calcification and intimal endothelial proliferation that leads to rapid and successive thrombosis and necrosis.
References
No comments:
Post a Comment