Prevalence at birth for EEC is reported at 1/10,000. Epispadias (E), classic bladder exstrophy (CEB) and EC are recognized clinical variants of the same spectrum, so accurate epidemiological data on E/EC/CEB are no longer available. The male-to-female ratio varies between studies; male or female predominance and a sex ratio close to unity have been described.
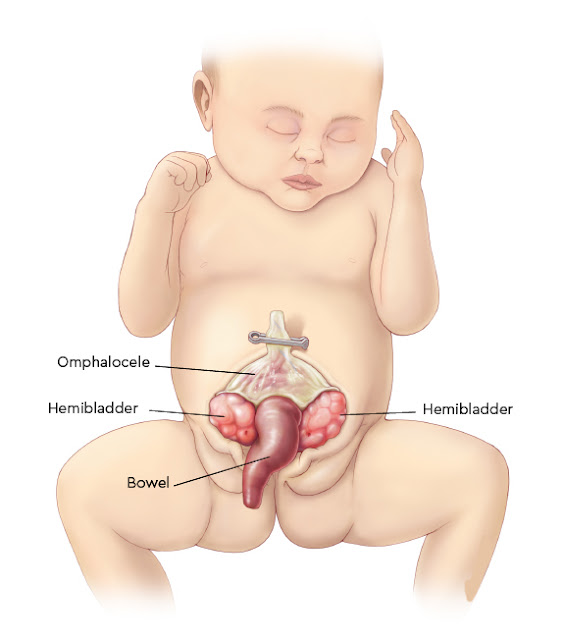
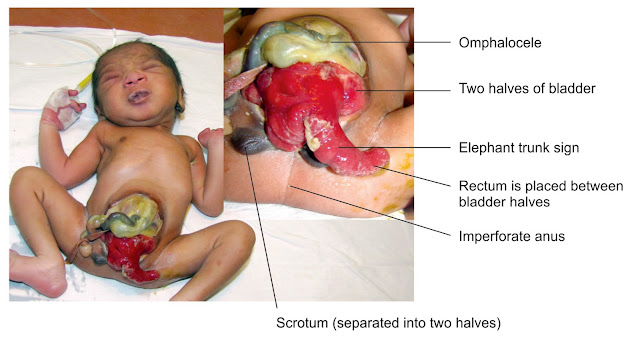
Patients present at birth with two exstrophied hemibladders separated by a foreshortened hindgut (often blind-ending resulting in an imperforate anus) or cecum. Omphalocele is found in 88-100% of patients and gastrointestinal (GI) malrotation/duplication and short bowel syndrome (see this term) are present in 46%, with absorptive dysfunction in some cases. The symphysis pubis is widely separated and the pelvis is often asymmetrically shaped. The genitalia, e.g. the penile or clitoral halves, can be located separately on either side of the bladder plates with the adjacent scrotal or labial part.
📖 Lippincott’s Illustrated Q and A Review of Anatomy and Embryology
Duplication of the vagina and uterus, as well as vaginal agenesis, has also been reported. Various urological malformations (ureteropelvic junction obstruction, ectopic pelvic kidney, horseshoe kidney, renal hypo- or agenesis, megaureter, ureteral ectopy and ureterocele) may also be present. Spinal abnormalities ranging from hemivertebra to myelomeningocele occur in all patients and may be accompanied by skeletal and limb anomalies (clubfoot deformities, absence of feet, tibial/fibular deformities, and hip dislocation).
 |
| Cloacal exstrophy |
EC results from an anomaly during early embryologic development associated with rupture of the cloacal membrane before fusion with the urorectal septum. The underlying cause remains unknown: genetic and environmental factors are likely to play a role.
Diagnosis is evident at birth but spinal ultrasound and radiographs, MRI and urogenital ultrasound are recommended to determine the nature and extent of the malformations, with laboratory tests to detect electrolyte losses from the terminal ileum.
Prenatal diagnosis is possible from ultrasound findings (non-visualization of the bladder, anterior wall defects, omphalocele and myelomeningocele are major criteria). Prenatal diagnosis should lead to parental counseling to provide information on the nature of the malformation and the extent of surgical reconstruction required. However, termination of pregnancy should not be automatically indicated.
Patients require immediate postnatal multidisciplinary care followed by surgical management, usually beginning in the newborn period with immediate closure of the meningocele and omphalocele as well as adaptation of bladder halves. Later, a multistage approach for bladder and bowel reconstruction is used, including a mandatory osteotomy due to severe pelvic asymmetry and the large ventral defect. The main aims of management are secure abdominal wall closure, prevention of short bowel syndrome, urinary and fecal continence, preserved renal function, and adequate cosmetic and functional genital reconstruction. Multiple associated anomalies have to be considered to achieve successful reconstruction.
Surgical advances and improved neonatal care have led to a dramatic increase in survival rates and improvements in continence rates and therefore quality of life. However, patients require life-long follow up, including psychosocial and psychosexual aspects, from a multidisciplinary team of experts.
References
No comments:
Post a Comment