Kahler’s disease (Multiple myeloma), the most common bone malignancy, is occurring with increasing frequency in older persons. Typical symptoms are bone pain, malaise, anemia, renal insufficiency, and hypercalcemia. Incidental discovery on comprehensive laboratory panels is common. The disease is diagnosed with serum or urine protein electrophoresis or immunofixation and bone marrow aspirate analysis.
 |
| Kahler’s disease |
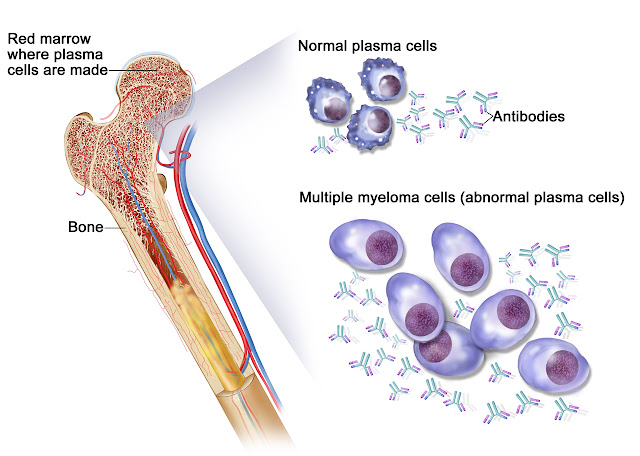
On the picture: Kahler’s disease. Kahler’s disease cells are abnormal plasma cells (a type of white blood cell) that build up in the bone marrow and form tumors in many bones of the body. Normal plasma cells make antibodies to help the body fight infection and disease. As the number of Kahler’s disease cells increases, more antibodies are made. This can cause the blood to thicken and keep the bone marrow from making enough healthy blood cells. Kahler’s disease cells also damage and weaken the bone.
Skeletal radiographs are important in staging Kahler’s disease and revealing lytic lesions, vertebral compression fractures, and osteoporosis. Magnetic resonance imaging and positron emission tomography or computed tomography are emerging as useful tools in the evaluation of patients with myeloma; magnetic resonance imaging is preferred for evaluating acute spinal compression. Nuclear bone scans and dual energy x-ray absorptiometry have no role in the diagnosis and staging of myeloma. The differential diagnosis of monoclonal gammopathies includes monoclonal gammopathy of uncertain significance, smoldering (asymptomatic) and symptomatic Kahler’s disease, amyloidosis, B-cell non-
 |
| Characteristic osteolytic lesions in the skull of a patient with myeloma |
Hodgkin lymphoma, Waldenström macroglobulinemia, and rare plasma cell leukemia and heavy chain diseases. Patients with monoclonal gammopathy of uncertain significance or smoldering Kahler’s disease should be followed closely, but not treated.
📖 Cancer, Principles and Practice of Oncology
Symptomatic Kahler’s disease is treated with chemotherapy followed by autologous stem cell transplantation, if possible. Melphalan, prednisolone, dexamethasone, vincristine, doxorubicin, bortezomib, and thalidomide and its analogue lenalidomide have been used successfully. It is important that family physicians recognize and appropriately treat Kahler’s disease complications. Bone pain is treated with opiates, bisphosphonates, radiotherapy, vertebroplasty, or kyphoplasty; nephrotoxic nonsteroidal anti-inflammatory drugs should be avoided. Hypercalcemia is treated with isotonic saline infusions, steroids, furosemide, or bisphosphonates. Because of susceptibility to infections, patients require broad-spectrum antibiotics for febrile illness and immunization against influenza, pneumococcus, and Haemophilus influenzae B. Five-year survival rates approach 33 percent, and the median survival rate is 33 months.
 |
Bone marrow aspirate cytology of multiple myeloma, a type of bone marrow cancer of malignant plasma cells, associated with bone pain, bone fractures and anemia. |
Kahler’s disease is the most common primary bone malignancy. More than 50,000 persons in the United States are currently diagnosed with Kahler’s disease, and 16,000 are diagnosed annually. As the population ages, it is important for family physicians to diagnose myeloma and recognize its many complications.
Many
patients with Kahler’s disease initially present with unexplained backache or
bone pain. The long bones, ribs, skull, and pelvis are also commonly involved,
and most patients have multiple lytic skeletal lesions. Pathologic fracture is
the presenting symptom in 26 to 34 percent of patients. Vertebral compression
fractures can lead to weakness and paresthesias in the lower extremities.
Carpal tunnel syndrome is the most common peripheral neuropathy in patients
with Kahler’s disease. Anorexia, nausea, somnolence, and polydipsia are common
symptoms of hypercalcemia. Weakness and malaise are usually associated with Kahler’s
disease anemia. Impaired antibodies and leukopenia cause recurrent infections,
usually from encapsulated organisms (pneumonia is the most common infection).
Weight loss occurs in less than one fourth of patients, and fever is rare at
presentation.
The diagnostic criteria for smoldering (asymptomatic) multiple myeloma is a serum M protein level of 3 g per dL (30 g per L) or more, 10 percent or more bone marrow plasma cells, and no related organ or tissue impairment (i.e., no end-organ damage, including bone lesions) or symptoms. The diagnostic criteria for symptomatic multiple myeloma is M protein (serum or urine), bone marrow clonal plasma cells or plasmacytoma, and myeloma-related organ or tissue impairment. Patients with symptoms suggestive of multiple myeloma (e.g., unexplained weakness, fatigue, back pain, proteinuria, anemia, renal insufficiency, recurrent infections, peripheral neuropathy) should be screened with serum and urine protein electrophoresis.
Serum and urine protein immunofixation are also recommended because immunofixation can be diagnostic even with a normal or nonspecific protein electrophoretic pattern. Urine dipstick tests are insensitive for Bence Jones protein, and urine protein electrophoresis and immunofixation are recommended in all patients with plasma cell dyscrasias. Bone marrow aspirate analysis should be performed in patients with abnormal serum or urine proteins and may require multiple samples because findings may be focal.
Kahler’s
disease anemia is typically normochromic and normocytic, although macrocytosis
with vitamin B12 deficiency has been reported. Only 10 to 15 percent of
patients have thrombocytopenia, and even fewer have leukocytosis—both
conditions reflect severe plasma cell infiltration of the bone marrow. A
complete blood count showing circulating plasma cells is uncommon, unless the
disease is advanced. Sedimentation rates are typically greater than 50 mm per
hour, although patients with Bence Jones myeloma often have values of less than
20 mm per hour.
There is no standard imaging work-up for Kahler’s disease, but a skeletal radiograph survey is generally recommended.6 Because radiography can take time, many institutions use whole-body radiographs with C-arm instruments designed for five-minute trauma scans. Lytic lesions are evident on radiography when 50 percent or more of trabecular bone is lost. The lesions appear on radiography even after successful treatment of Kahler’s disease. Magnetic resonance imaging (MRI) is the preferred technique for suspected spinal compression or soft-tissue plasmacytomas. Computed tomography (CT) alone is more sensitive than plain radiography for small long bone lesions and can differentiate malignant from benign vertebral compression fractures in patients who are not MRI candidates. However, CT is not typically recommended for initial skeletal surveying. Although positron emission tomography with CT is not the standard of care, it is being used for staging and follow-up. Dual energy x-ray absorptiometry has no role in diagnosing Kahler’s disease, and nuclear bone scans are not helpful because of the lack of osteoblastic activity.
Otto Kahler (1849 - 1893), Austrian internist.
 |
| Otto Kahler |
Otto Kahler, the son of a physician, studied in his native city of Prague and obtained his doctorate in 1871. Following an educational journey to Paris, Kahler became assistant at the internal clinic of Joseph Halla (1814-1887) in Prague, and was habilitated as Dozent for internal medicine at the German university in Prague, becoming ausserordentlicher professor in 1882, 1886 ordinarius of special pathology and therapy and head of the 2nd medical clinic at the German university.
Kahler preached the gospel of Jean-Martin Charcot’s (1825-1893) approach to clinical medicine and neurology to Middle Europe. When in 1889 he moved to Vienna to succeed Heinrich von Bamberger (1822-1888) as ordinarius of special pathology and head of the medical clinic, he took Friedrich Kraus (1858-) with him as assistant.
After a year in Vienna Kahler developed cancer of the tongue. Kraus took over his lectures and established himself as a brilliant teacher, laying the foundation for his appointment to Berlin. Kahler died in Vienna in 1893.
Despite his short lifespan, by his literary activity Kahler obtained a reputation as one of the important clinicians in his time.
References
No comments:
Post a Comment