Prader-Labhart-Willi Syndrome is a complex, multisystem sporadic disorder which presents during childhood and proceeds into adulthood.
 |
| Prader-Labhart-Willi syndrome |
The major features include infantile hypotonia, developmental delay, hypogonadism with abnormal sexual maturation, mental retardation and behavior abnormalities, short stature with small hands and feet, massive obesity with diabetes mellitus, dysmorphic facial features, and marked dental caries and enamel hypoplasia. Recently, a deletion of chromosome 15 has been found in a large percentage of these patients, but the exact cause and genetic transmission has not yet been determined.
 |
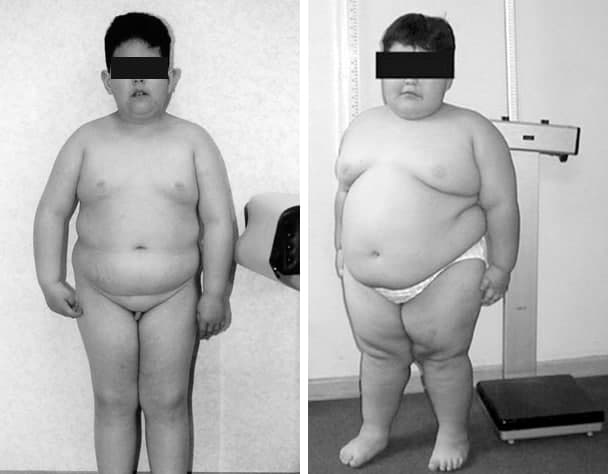
7-year-old boy with obesity, short stature, characteristic shape of the mouth, acromicria, genua valgum, and hypogonadism has Prader-Labhart-Willi syndrome. |
First described in 1956 by A. Prader, A. Labhart, and H. Willi, all three Swiss pediatricians and internists, on the basis of observation obtained from nine children with the tetrad of short stature, mental retardation, severe obesity, and small hands and feet. In 1961, muscle hypotonia in infancy was added to the phenotype. Diabetes mellitus usually develops in childhood.
In the United States, most cases are sporadic in occurrence. Rate of prevalence is reported to be 1:16,062 live births by Burd et al., whereas Butler et al. reports a prevalence of 1:25,000 live births. Internationally, the reported prevalence range from 1:8,000 in rural Sweden to 1:16,000 in western Japan.
Syndrome results from the loss of the paternal copy of chromosome 15q11.2-13. It is described as a microdeletion/disomy disorder. However, most cases arise sporadically. More than 70% of patients have a deletion of the paternal copy. Approximately 25% of patients have maternal uniparental disomy for chromosome 15. The remainder present with translocation or other structural aberration in chromosome 15.
Reduction in lung volumes, including expiratory reserve volume, vital capacity, and functional residual capacity; closing capacity is increased, leading to airway closure in the dependent areas of the lung and V/Q mismatch; reduced chest and diaphragmatic excursions; decreased alveolar ventilation; diminished sensitivity of the respiratory center to hypoxia and hypercarbia—all contributing to hypoxia and hypercarbia. Intermittent upper airway obstruction and hypoxia during sleep with resultant chronic sleep deprivation and daytime somnolence; severe and chronic hypoxia leading to polycythemia, pulmonary hypertension, right ventricular hypertrophy, and failure.
Neonatal hypotonia is one hallmark feature of this disorder and is a valuable clue to initiate diagnostic testing. Clinical features; biochemical (polycythemia, hypoxia, hypercarbia); lung function tests (reduced lung volumes including total lung capacity, functional residual capacity, vital capacity, and expiratory reserve volume); ECG (right axis deviation); chest radiograph or echocardiography (cardiomegaly); sleep studies (obstructive sleep apnea).
The syndrome is biphasic; initially the picture is one of hypotonia and later changes to hyperphagia leading to obesity.
Antenatal: delayed onset and reduced fetal activity during pregnancy; often breech presentation at birth.
Neonatal and infancy: low birth weight, infantile hypotonia (“floppy infant”), neonatal asphyxia, poor feeding, and failure to thrive; gross motor developmental delay, weak cry and cough, hypogonadism with genital hypoplasia. Neonates may require tube feeding for 3 to 4 months, although this usually improves by 6 months and by 12 to 18 months, uncontrollable hyperphagia occurs.
 |
| Andrea Prader, Alexis Labhart, Heinrich Willi |
Andrea Prader, in collaboration with Heinrich Willi, the head of the newborn nursery, and Alexis Labhart, an endocrinologist in private practice, identified 8 other cases, all younger than Albert.
They published their paper in 1956, with Prader as the first author. The syndrome was initially called Prader-Labhart-Willi syndrome (PLWS) and the name changed to Prader-Willi syndrome (PWS). Though Labhart was eventually dropped from the name of the syndrome, Prader always insisted on recognizing Labhart’s role.
Discovering the syndrome was a huge achievement, but it was not recognized as such at the time. The paper was published in a small Swiss journal, in German. In the 1960s, other doctors began to investigate, but they still didn’t know what caused the obesity. The majority view was simply that they were eating too much.
After eight years in Beirut, Zellweger moved to the University of Iowa in 1959. He began diagnosing PWS in his patients and by the late 1960s, he had 14 cases. He noted they had “deficient control of their emotions. They show exuberant feelings of joy and pleasure…they can also be extremely stubborn.”
It was not until 1972 that a review of PWS was published in The Journal of Pediatrics, a publication widely read by pediatricians. As recently as 60 to 70 years ago, many families did not know what to do with children like these and a common solution was to give them up to be raised by an institution. Even in the 1970s, the medical literature had nothing good in it for families of children with this syndrome.
Dr. Andrea Prader came to the United States in 1984 to attend the PWSA | USA conference in Minneapolis, MN. He visited the residents at Oakwood and was impressed by the conference and PWSA | USA. He said, “You were the first Prader-Willi syndrome association in the world bringing together parents, doctors, other health workers and teachers. It is one of the most admirable qualities of American people, to develop very powerful private initiative; to have a strong will to help each other; not to be ashamed to have a so-called abnormal child and to go public in support of these children.” The International Organisation of Prader-Willi Syndrome (IPWSO) would not be formed for another 30 years, and was formed by the scientific community, unlike PWSA | USA’s early parents.
Hans Zellweger died in 1990 at the age of 80. He took his own life. Zellweger, who had shown so much compassion and understanding for people with PWS and their families held himself to a harsher standard.
Andrea Prader died in 2001 at the age of 81. Like Zellweger, his final years were not easy. After losing his wife of nearly 50 years in 1995, he lost his zest and curiosity for science. But despite the sad ending, he had accomplished what he set out to do in life: make scientific discoveries. Besides discovering Prader-Willi syndrome, he discovered several inborn errors of metabolism and became a worldwide leader in the study of growth and puberty.
Alexis Labhart died in 1994 at the age of 78. Heinrich Willi died in 1971 at the age of 71.
References
1: Cassidy SB, Schwartz S, Miller JL, Driscoll DJ. Prader-Willi syndrome. Genet
Med. 2012 Jan;14(1):10-26. doi: 10.1038/gim.0b013e31822bead0. Epub 2011 Sep 26.
PMID: 22237428.
2: Butler MG, Miller JL, Forster JL. Prader-Willi Syndrome - Clinical Genetics,
Diagnosis and Treatment Approaches: An Update. Curr Pediatr Rev.
2019;15(4):207-244. doi: 10.2174/1573396315666190716120925. PMID: 31333129;
PMCID: PMC7040524.
3: Angulo MA, Butler MG, Cataletto ME. Prader-Willi syndrome: a review of
clinical, genetic, and endocrine findings. J Endocrinol Invest. 2015
Dec;38(12):1249-63. doi: 10.1007/s40618-015-0312-9. Epub 2015 Jun 11. PMID:
26062517; PMCID: PMC4630255.
4: Abdilla Y, Andria Barbara M, Calleja-Agius J. Prader-Willi Syndrome:
Background and Management. Neonatal Netw. 2017 May 1;36(3):134-141. doi:
10.1891/0730-0832.36.3.134. PMID: 28494825.
5: Krasińska A, Skowrońska B. [Prader-Willi Syndrome - nutritional management in
children, adolescents and adults]. Pediatr Endocrinol Diabetes Metab.
2017;23(2):101-106. Polish. doi: 10.18544/PEDM-23.02.0080. PMID: 29073293.
6: Passone CBG, Pasqualucci PL, Franco RR, Ito SS, Mattar LBF, Koiffmann CP,
Soster LA, Carneiro JDA, Cabral Menezes-Filho H, Damiani D. PRADER-WILLI
SYNDROME: WHAT IS THE GENERAL PEDIATRICIAN SUPPOSED TO DO? - A REVIEW. Rev Paul
Pediatr. 2018 Jul-Sep;36(3):345-352. doi: 10.1590/1984-0462/;2018;36;3;00003.
PMID: 30365815; PMCID: PMC6202899.
7: Alves C, Franco RR. Prader-Willi syndrome: endocrine manifestations and
management. Arch Endocrinol Metab. 2020 May-Jun;64(3):223-234. doi:
10.20945/2359-3997000000248. PMID: 32555988.
8: Duis J, van Wattum PJ, Scheimann A, Salehi P, Brokamp E, Fairbrother L,
Childers A, Shelton AR, Bingham NC, Shoemaker AH, Miller JL. A multidisciplinary
approach to the clinical management of Prader-Willi syndrome. Mol Genet Genomic
Med. 2019 Mar;7(3):e514. doi: 10.1002/mgg3.514. Epub 2019 Jan 29. PMID:
30697974; PMCID: PMC6418440.
9: Donzelli O, Nanni ML, Terzi S, Iantorno DM. Prader-Willi-Labhart syndrome:
orthopaedic complications. Chir Organi Mov. 1993 Oct-Dec;78(4):241-6. English,
Italian. PMID: 8149785.
10: Cassidy SB. Prader-Willi syndrome. J Med Genet. 1997 Nov;34(11):917-23. doi:
10.1136/jmg.34.11.917. PMID: 9391886; PMCID: PMC1051120.
Tags: prader labhart willi syndrome, prader labhart willi fanconi syndrome, what is the life expectancy of prader-willi syndrome, what is the life expectancy of someone with prader willi syndrome, what is the life expectancy of a person with prader willi syndrome, what is the life expectancy of a child with prader willi syndrome, prader-willi syndrome, prader willi syndrome undiagnosed, prader willi syndrome effects, prader-willi syndrome cause, syndrome de prader-labhart-willi, que es el sindrome de prader willi, que es sindrome de prader willi, undiagnosed prader willi syndrome, prader willi disorder, diagnosis prader willi syndrome, prader willi syndrome cause of death, prader willi syndrome female, prader willi syndrome description, prader willi syndrome child, severe prader willi syndrome, prader willi syndrome types, prader willi syndrome detection, prader willi syndrome quiz, prader willi diagnosis, what's prader willi syndrome, william prader willi syndrome, prader willi syndrome spectrum


No comments:
Post a Comment