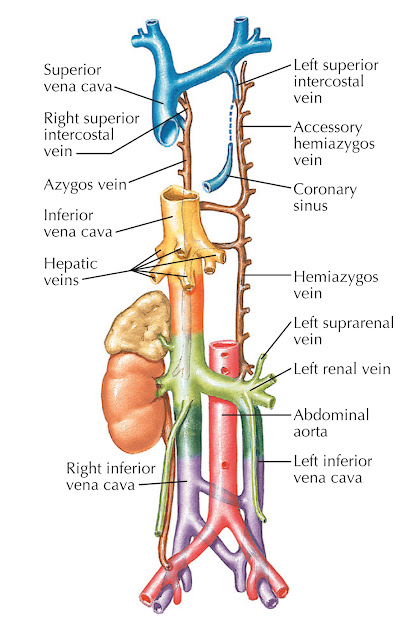
Double inferior vena cava is a vein abnormality that is present from birth (congenital). Individuals with this anomaly have two inferior vena cavas instead of one. The inferior vena cava carries oxygen-poor blood from the lower parts of the body into the heart. Double inferior vena cava does not cause any symptoms. It is usually diagnosed when an imaging test, such as CT or MRI, is performed for other medical reasons. The reported incidence of double inferior vena cava ranges from 0.2 percent to 3 percent
 |
| Double inferior vena cava |
A double or duplicated inferior vena cava results from lack of atrophy in part of the left supracardinal vein, resulting in a duplicate structure to the left of the aorta. The common form is a partial paired inferior vena cava that connects the left common iliac and left renal veins. When caval interruption, such as placement of a filter, is planned, these alternate pathways must be considered. As an alternative, the inferior vena cava may not develop. The most common alternate route for blood flow is through the azygous vein, which enlarges to compensate. If a venous stenosis is present at the communication of iliac veins and azygous vein, back pressure can result in insufficiency, stasis, or thrombosis.