Babington’s disease - Osler-Weber-Rendu syndrome (OWR) is also known as hereditary hemorrhagic telangiectasia (HHT). It’s a genetic blood vessel disorder that often leads to excessive bleeding. According to the HHT Foundation International, the syndrome affects about one in 5,000 people. However, many people with the disease don’t know they have it, so this number may actually be higher.
 |
| Babington’s disease |
The name Osler-Weber-Rendu syndrome is named for the doctors who worked on researching this condition in the 1890s. They discovered that issues with blood clotting don’t cause this condition, which was previously assumed. Instead, this condition is caused by problems with the blood vessels themselves.
 |
Babington’s disease
| |
📖
Clinical Dermatology – A Color Guide to Diagnosis and Therapy, 6e In a healthy circulatory system, there are three types of blood vessels. There are arteries, capillaries, and veins. Blood moving away from your heart is carried through arteries, which travels at a high pressure. Blood moving towards your heart is carried through veins, and it travels at a lower pressure. The capillaries sit between these two types of blood vessels, and the narrow passageway of your capillaries helps to lower the pressure of the blood before it reaches the veins.
People with OWR are missing capillaries in some of their blood vessels. These abnormal blood vessels are known as arteriovenous malformations (AVM).The most characteristic lesions of hereditary hemorrhagic telangiectasia are small red-to-violet telangiectatic lesions on the face, lips, oral and nasal mucosa, and tips of the fingers and toes. Similar lesions may be present throughout the mucosa of the gastrointestinal (GI) tract, resulting in recurrent GI bleeding. Patients may experience recurrent, profuse nosebleeds. Some patients have pulmonary arteriovenous malformations (AVMs). These AVMs may cause significant right-to-left shunts, which can result in dyspnea, fatigue, cyanosis, or erythrocytosis. However, the first sign of the presence of AVMs may be a brain abscess, transient ischemic attack, or stroke as a result of infected or noninfected emboli. Cerebral or spinal AVMs occur in some families and may cause subarachnoid hemorrhage, seizures, or paraplegia. Hepatic AVMs may lead to liver failure and high output heart failure. Chronic iron deficiency anemia is commonly present.
Benjamin Guy Babington (1794 - 1866), English physician.
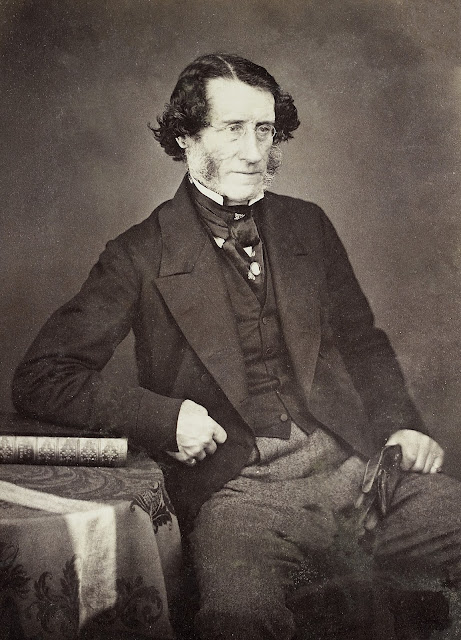 |
| Benjamin Guy Babington |
Benjamin Guy Babington was the son of the physician William Babington (1756-1833). He was educated at Charterhouse before joining the Royal Navy, serving as midshipman at the Battle of Copenhagen in 1891 as well as at Walcheren.
In 1812, after two years of study at the East India Company's college at Haileybury, Hertfordshire, he entered the Indian service at the presidency of Madras. He obtained such a thorough understanding of Oriental languages and Sanskrit, that already at the age of twenty he was able to publish the first grammar of the Indian language Tanul.
Babington health suffered from the Indian climate, however, and he returned to England. He then studied medicine at Guy's Hospital, London, and Pembroke College, Cambridge, receiving his doctorate from the latter in 1831. He later became a fellow of the College of Physicians.
When cholera first came to England in 1832, he conducted investigations into it and was the first in England to describe the exanthema that is observed with cholera.
In 1837 Babington became assistant physician, at Guy's - ahead of Hodgkin. This aroused a great deal of controversy and acrimonious debate. The treasurer of the hospital said he would have no one at Guy's hospital that was seen in the company of a North American Indian - a reference to Hodgkin's well-known liberal tendencies - he was a founder of the Aborigine Society.
Babington was also probably helped by his family connections; his father had been a physician at Guy's and his sister was Richard Bright's first wife. Babington resigned from Guy's in 1855 following a disagreement with the hospital administration over restriction of access of students to the hospital.
Babington was a member of the board of the Royal Society, and in his quality as member of the Medical Council of the General Board of Health, received several government assignments in investigations. In 1863 he was also president of the Royal Medical and Chirurgical Society. Having become convinced of the importance of research in epidemics, he in 1850 became founder of the Epidemiological Society, of which he was chairman for many years, and published several valuable papers in its transactions.
Babington was a man of many talents; a skilled sculptor and painter, as well as a linguist and translator of verse; a fine billiard player and a good shot. To Babington, furthering science was more important than gaining personal fame. He was an amiable, sociable character, as well as a highly skilled physician, familiar with all the possibilities available to medical science.
He was one of the first to put Victor Théodore Junod's (1809-1881) hemopsy to use, and invented a curved stethoscope, a hygrometer. He was very clever in using mirrors for investigations of the throat. In 1828 he invented an instrument, which he called the glottiscope for examining the larynx - the first laryngoscope. He was the first to introduce routine indirect laryngoscopy. He wrote on cholera, epilepsy and chorea, and was one of the first to suggest that fibrin was formed in the blood from a more soluble precursor. He died from renal and bladder disease on April 8, 1866.
Well versed in foreign languages, Babington took an interest in translations, and 1833-1836 published four papers from J. F. K. Hecker’s Epidemics of the Middle Ages, which was later expanded, and published by the Sydenham Society. He also published Baron Ernst Von Feuchtersleben’s (1806-1849) Principles of Medical Psychology.
References
1: Orizaga-Y-Quiroga TL, Villarreal-Martínez A, Jaramillo-Moreno G, Ocampo-
Candiani J. Osler-Weber-Rendu Syndrome in Relation to Dermatology. Actas
Dermosifiliogr. 2019 Sep;110(7):526-532. English, Spanish. doi:
10.1016/j.ad.2018.11.007. Epub 2019 Apr 8. PMID: 30975431.
2: Tortora A, Riccioni ME, Gaetani E, Ojetti V, Holleran G, Gasbarrini A. Rendu-
Osler-Weber disease: a gastroenterologist's perspective. Orphanet J Rare Dis.
2019 Jun 7;14(1):130. doi: 10.1186/s13023-019-1107-4. PMID: 31174568; PMCID:
PMC6555961.
3: Benítez-Rivero S, Camacho Romero J, Eiroa D. Rendu-Osler-Weber syndrome. Med
Clin (Barc). 2019 Jun 7;152(11):e65. English, Spanish. doi:
10.1016/j.medcli.2018.07.016. Epub 2018 Nov 2. PMID: 30392695.
4: Butt MU, Yoo E, Khan U. Osler-Weber-Rendu syndrome. QJM. 2016
Sep;109(9):615-6. doi: 10.1093/qjmed/hcw094. Epub 2016 Jun 17. PMID: 27318363.
5: Watad A, Belsky V, Shoenfeld Y, Amital H. Osler-Weber-Rendu Syndrome. Isr Med
Assoc J. 2015 May;17(5):328. PMID: 26137666.
6: Jolobe OMP. Underuse of screening in Osler-Weber-Rendu syndrome. QJM. 2017
May 1;110(5):337. doi: 10.1093/qjmed/hcw221. PMID: 28087692.
7: Cohn JE, Scharf J. Telangiectasias in Osler-Weber-Rendu Syndrome. Otolaryngol
Head Neck Surg. 2017 Jul;157(1):162-163. doi: 10.1177/0194599817702876. Epub
2017 Apr 18. PMID: 28417691.
8: Morphet JA. Osler-Weber-Rendu syndrome. CMAJ. 2006 Nov 7;175(10):1243. doi:
10.1503/cmaj.1060182. PMID: 17098956; PMCID: PMC1626522.
9: Abangah G, Rashidbeygi M. Osler-Weber-Rendu syndrome. BMJ Case Rep. 2013 Oct
9;2013:bcr2013201034. doi: 10.1136/bcr-2013-201034. PMID: 24108772; PMCID:
PMC3822155.
10: Borovac-Pinheiro A, Cavichiolli FS, Costa ML, Surita FG. Osler-Weber-Rendu
syndrome in pregnancy affecting lungs and brain-a case report. J Obstet
Gynaecol. 2019 Jul;39(5):709-711. doi: 10.1080/01443615.2019.1581739. Epub 2019
Apr 25. PMID: 31020882.


No comments:
Post a Comment