 |
| Prader-Labhart-Willi syndrome |
 |
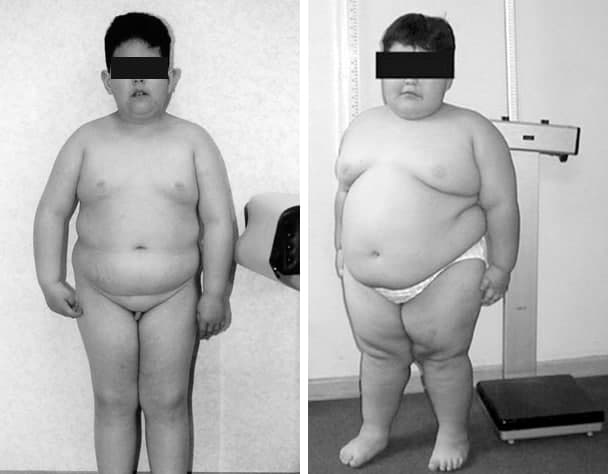
7-year-old boy with obesity, short stature, characteristic shape of the mouth, acromicria, genua valgum, and hypogonadism has Prader-Labhart-Willi syndrome. |
 |
| Prader-Labhart-Willi syndrome |
 |
7-year-old boy with obesity, short stature, characteristic shape of the mouth, acromicria, genua valgum, and hypogonadism has Prader-Labhart-Willi syndrome. |
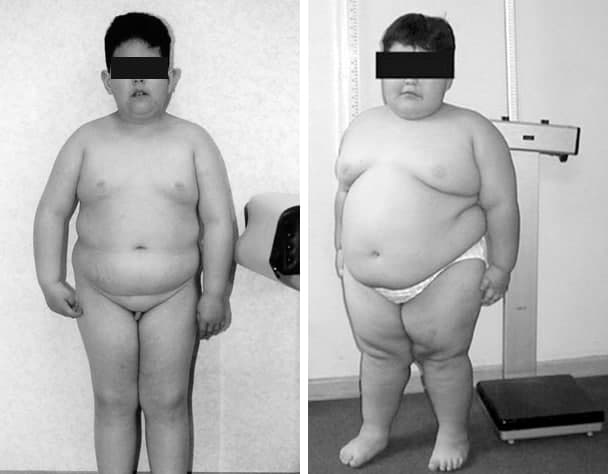
Kahler’s disease (Multiple myeloma), the most common bone malignancy, is occurring with increasing frequency in older persons. Typical symptoms are bone pain, malaise, anemia, renal insufficiency, and hypercalcemia. Incidental discovery on comprehensive laboratory panels is common. The disease is diagnosed with serum or urine protein electrophoresis or immunofixation and bone marrow aspirate analysis.
 |
| Kahler’s disease |
On the picture: Kahler’s disease. Kahler’s disease cells are abnormal plasma cells (a type of white blood cell) that build up in the bone marrow and form tumors in many bones of the body. Normal plasma cells make antibodies to help the body fight infection and disease. As the number of Kahler’s disease cells increases, more antibodies are made. This can cause the blood to thicken and keep the bone marrow from making enough healthy blood cells. Kahler’s disease cells also damage and weaken the bone.
Skeletal radiographs are important in staging Kahler’s disease and revealing lytic lesions, vertebral compression fractures, and osteoporosis. Magnetic resonance imaging and positron emission tomography or computed tomography are emerging as useful tools in the evaluation of patients with myeloma; magnetic resonance imaging is preferred for evaluating acute spinal compression. Nuclear bone scans and dual energy x-ray absorptiometry have no role in the diagnosis and staging of myeloma. The differential diagnosis of monoclonal gammopathies includes monoclonal gammopathy of uncertain significance, smoldering (asymptomatic) and symptomatic Kahler’s disease, amyloidosis, B-cell non-
 |
| Characteristic osteolytic lesions in the skull of a patient with myeloma |
Hodgkin lymphoma, Waldenström macroglobulinemia, and rare plasma cell leukemia and heavy chain diseases. Patients with monoclonal gammopathy of uncertain significance or smoldering Kahler’s disease should be followed closely, but not treated.
The antiglobulin, or Coombs test is part of the compatibility tests that any patient who will receive a red blood cell transfusion must undergo. This test is also essential in the diagnostic work of patients with anemia whose origin is not easily determined and when the etiology must be identified precisely.
 |
| Direct Coombs test |
In 1945, Robin Coombs, Arthur Mourant and Rob Race described a test to detect anti-Rho (anti-D) non-agglutinant antibodies. Originally, the test was devised by Robin Coombs as part of his postgraduate studies at Race and Mourant's laboratory in Cambridge, England in 1945. His goal was to study the characteristics of the antibodies involved in the context of what was known as fetal erythroblastosis, which is now known as hemolytic disease of the newborn (HDN), caused most frequently by the incompatibility between an Rh-negative mother sensitized during a previous pregnancy, who produces IgG anti-D antibodies able to pass the placenta barrier due to their small size that then cover the fetal red blood cells.
 |
| Indirect Coombs test |
These are later phagocytosed in the spleen and liver, organs which, in addition to their other functions, maintain extramedullary hematopoiesis in the fetus to compensate for anemia resulting from hemolysis. Later, the Coombs test was used to demonstrate the presence of incomplete antibodies which covered the erythrocytes in vivo, such as is seen in cases of autoimmune hemolytic anemia (AHA). The description of the method, and its application in various hematological diseases, was published in The Lancet and The British Journal of Experimental Pathology in 1945 and 1946, respectively.
Marchiafava-Bignami disease (MBD) is a very rare disorder of demyelination/necrosis of the corpus callosum and the near subcortical white matter that is especially predominant in ill-fed alcoholics. It was discovered in 1903 by Italian pathologists Ettore Marchiafava and Amico Bignami. They described men with alcohol use disorder who died of seizures and coma that presented necrosis of their corpus callosum on autopsy. However, few cases have been described in non-alcoholic patients, suggesting that alcohol is not the sole responsible for these lesions.
 |
| Marchiafava-Bignami disease |
A, Parasagittal MR T1-weighted image shows multiple areas of decreased signal intensity involving the genu and the anterior aspect of the corpus callosum.
B, MR T2-weighted image corresponding to A shows the lesions to be hyperintense and also some mild atrophy of the involved portions of the corpus callosum.
C, MR Axial T2-weighted image shows a mild degree of periventricular white matter hyperintensity, particularly in the region of the frontal horns of the lateral ventricle.
D, Axial T2-weighted image at the level of the centra semiovale shows a mild degree of periventricular white matter hyperintensities.
📖 Neurology Self-Assessment: A Companion to Bradley’s Neurology in Clinical Practice
The structure of the Pacinian corpuscle was described by Pacini (1835). It is widely distributed in mammals and is similar to the Herbst corpuscles found in birds. The Pacinian corpuscle is an ovoid structure about 1 mm in length and is easily seen by the naked eye in a number of locations such as the mesentery.
 |
| Pacini's corpuscles |
On microscopic examination, the lamellar structure of the corpuscle is evident, the lamellae giving an appearance which has been likened to a section through an onion. The corpuscle is innerv!lted by a myelinated sensory axon of medium diameter which terminates within the center of the corpuscle.