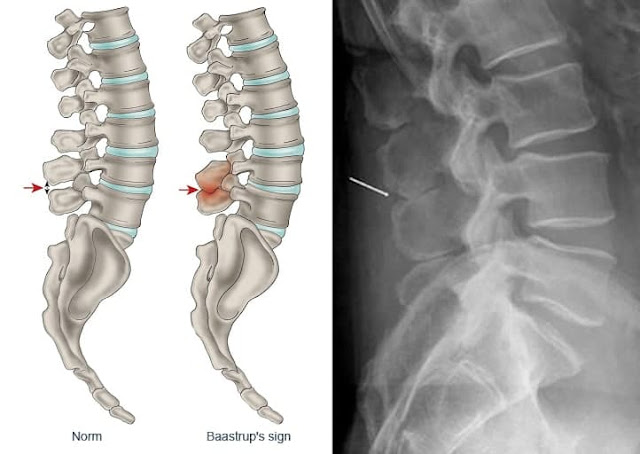
(Baastrup’s disease, Kissing spines syndrome)
Excessive lordosis is a common finding and may produce mechanical pressure that causes repetitive strains of the interspinous ligament with subsequent degeneration and collapse. Baastrup’s disease (kissing spine syndrome) is a term referring to close approximation of adjacent spinous processes due to degenerative changes of the spine.
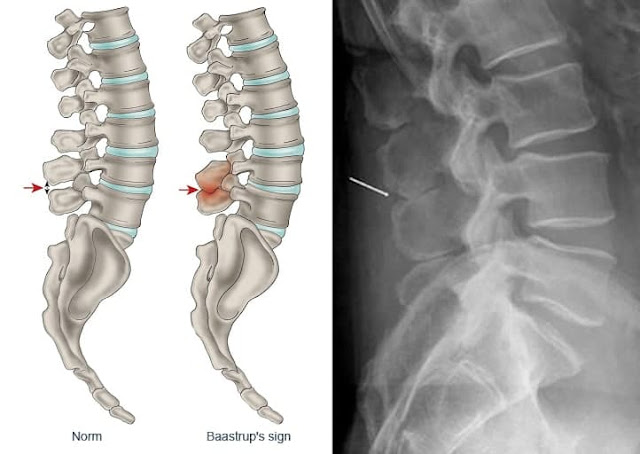 |
| Baastrup’s disease |
Baastrup’s disease usually affects the lumbar spine, with L4-L5 being the most commonly affected level. There is higher occurrence at ages over 70 and no gender predilection. Symptoms include back pain with midline distribution that worsens during extension, is relieved during flexion and is exaggerated upon finger pressure at the level of interest. Diagnosis rests on clinical examination and imaging studies. The hallmark of imaging findings is the close approximation and contact of adjacent spinous processes, with all the subsequent findings including oedema, cystic lesions, sclerosis, flattening and enlargement of the articulating surfaces, bursitis and occasionally epidural cysts or midline epidural fibrotic masses. Proposed therapies include conservative treatment, percutaneous infiltrations or surgical therapies such as excision of the bursa or osteotomy.
Pathogenesis
Baastrup’s disease is a term referring to close approximation of adjacent spinous processes due to general degenerative changes of the spine. Usually there is an excessive lordosis with resultant mechanical pressure process that causes repetitive strains of the interspinous ligament with subsequent degeneration and collapse.
📖 Practical Office Orthopedics