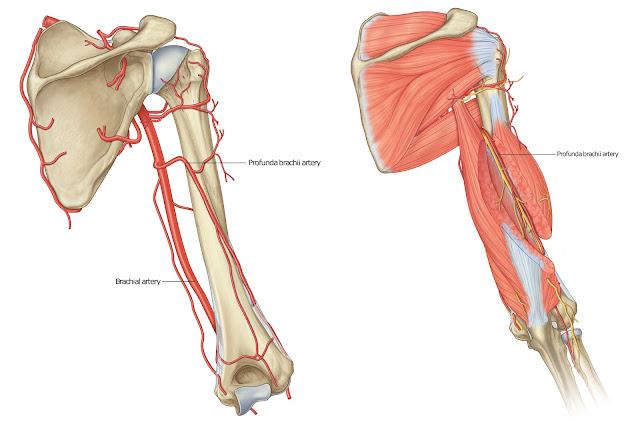
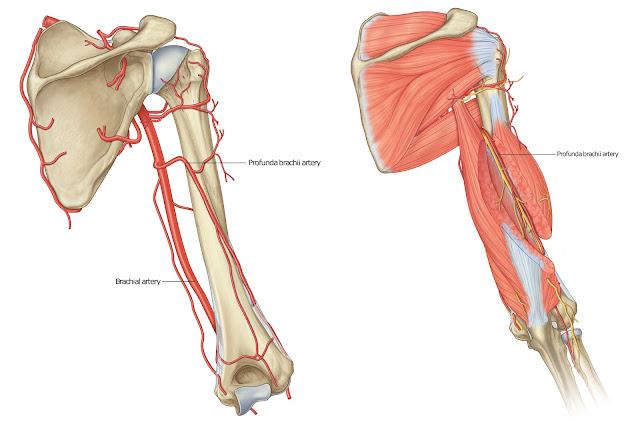
As a continuation of the axillary artery, it begins at the inferior border of the teres major tendon and it ends at the level of the neck of the radius about 1cm distal to the elbow joint. At this point, it divides into the ulnar and radial arteries. The brachial artery runs medial to the humerus proximally, before moving more anteriorly to lie between the epicondyles of the humerus.
 |
| Brachial artery |
Relationships of the brachial artery to other structures in the arm can be important in clinical practice. The brachial artery is a superficial vessel and is only covered by the layers of the skin, as well as the superficial and deep fasciae, with a few exceptions:
The first exception to this is at the cubital fossa, where the bicipital aponeurosis, which is the aponeurosis of the biceps brachii muscle, covers the artery, and separates it from the median cubital vein.
The second exception is when the median nerve crosses the brachial artery near the distal attachment of the coracobrachialis.
 |
| Brachial artery |
Posteriorly, the brachial artery is separated from the long head of the triceps brachii muscle by the profunda brachii artery and the radial nerve. The attachments of the coracobrachialis and the brachialis muscles, as well as the medial head of the triceps brachii muscle, also lie posterior to the brachial artery.
The median nerve and coracobrachialis muscle lie laterally to the brachial artery at its proximal aspect whereas the medial cutaneous nerve of the forearm and the ulnar nerve lie medially to the artery proximally.
📖 Clinically Oriented Anatomy 7th Edition