Saturday, March 27, 2021
Hemoglobin
Prader-Labhart-Willi syndrome
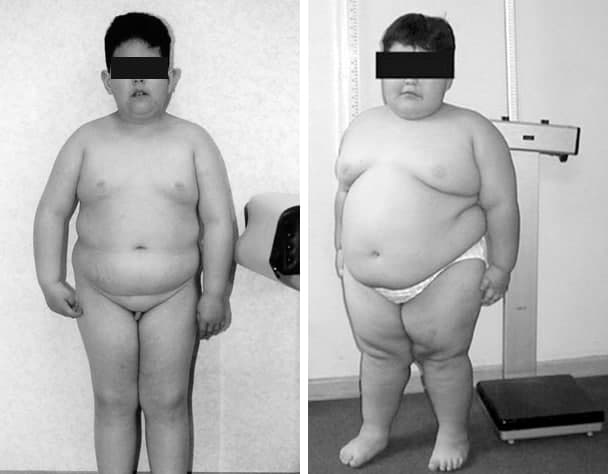 |
| Prader-Labhart-Willi syndrome |
 |
7-year-old boy with obesity, short stature, characteristic shape of the mouth, acromicria, genua valgum, and hypogonadism has Prader-Labhart-Willi syndrome. |
Wednesday, March 24, 2021
Kahler’s disease
Kahler’s disease (Multiple myeloma), the most common bone malignancy, is occurring with increasing frequency in older persons. Typical symptoms are bone pain, malaise, anemia, renal insufficiency, and hypercalcemia. Incidental discovery on comprehensive laboratory panels is common. The disease is diagnosed with serum or urine protein electrophoresis or immunofixation and bone marrow aspirate analysis.
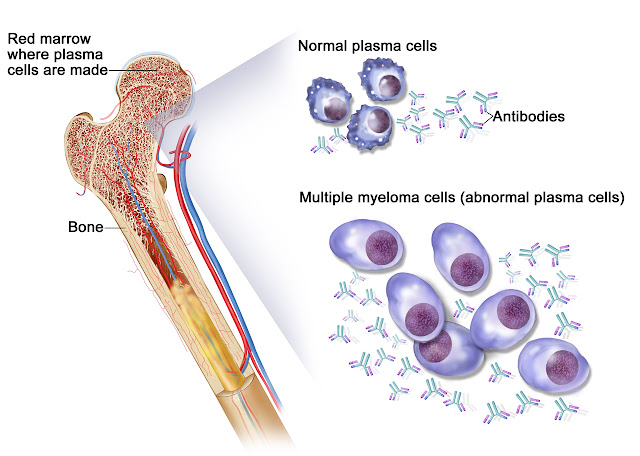 |
| Kahler’s disease |
On the picture: Kahler’s disease. Kahler’s disease cells are abnormal plasma cells (a type of white blood cell) that build up in the bone marrow and form tumors in many bones of the body. Normal plasma cells make antibodies to help the body fight infection and disease. As the number of Kahler’s disease cells increases, more antibodies are made. This can cause the blood to thicken and keep the bone marrow from making enough healthy blood cells. Kahler’s disease cells also damage and weaken the bone.
Skeletal radiographs are important in staging Kahler’s disease and revealing lytic lesions, vertebral compression fractures, and osteoporosis. Magnetic resonance imaging and positron emission tomography or computed tomography are emerging as useful tools in the evaluation of patients with myeloma; magnetic resonance imaging is preferred for evaluating acute spinal compression. Nuclear bone scans and dual energy x-ray absorptiometry have no role in the diagnosis and staging of myeloma. The differential diagnosis of monoclonal gammopathies includes monoclonal gammopathy of uncertain significance, smoldering (asymptomatic) and symptomatic Kahler’s disease, amyloidosis, B-cell non-
 |
| Characteristic osteolytic lesions in the skull of a patient with myeloma |
Hodgkin lymphoma, Waldenström macroglobulinemia, and rare plasma cell leukemia and heavy chain diseases. Patients with monoclonal gammopathy of uncertain significance or smoldering Kahler’s disease should be followed closely, but not treated.
Coombs test
The antiglobulin, or Coombs test is part of the compatibility tests that any patient who will receive a red blood cell transfusion must undergo. This test is also essential in the diagnostic work of patients with anemia whose origin is not easily determined and when the etiology must be identified precisely.
 |
| Direct Coombs test |
In 1945, Robin Coombs, Arthur Mourant and Rob Race described a test to detect anti-Rho (anti-D) non-agglutinant antibodies. Originally, the test was devised by Robin Coombs as part of his postgraduate studies at Race and Mourant's laboratory in Cambridge, England in 1945. His goal was to study the characteristics of the antibodies involved in the context of what was known as fetal erythroblastosis, which is now known as hemolytic disease of the newborn (HDN), caused most frequently by the incompatibility between an Rh-negative mother sensitized during a previous pregnancy, who produces IgG anti-D antibodies able to pass the placenta barrier due to their small size that then cover the fetal red blood cells.
 |
| Indirect Coombs test |
These are later phagocytosed in the spleen and liver, organs which, in addition to their other functions, maintain extramedullary hematopoiesis in the fetus to compensate for anemia resulting from hemolysis. Later, the Coombs test was used to demonstrate the presence of incomplete antibodies which covered the erythrocytes in vivo, such as is seen in cases of autoimmune hemolytic anemia (AHA). The description of the method, and its application in various hematological diseases, was published in The Lancet and The British Journal of Experimental Pathology in 1945 and 1946, respectively.
Tuesday, March 23, 2021
Marchiafava-Bignami disease
Marchiafava-Bignami disease (MBD) is a very rare disorder of demyelination/necrosis of the corpus callosum and the near subcortical white matter that is especially predominant in ill-fed alcoholics. It was discovered in 1903 by Italian pathologists Ettore Marchiafava and Amico Bignami. They described men with alcohol use disorder who died of seizures and coma that presented necrosis of their corpus callosum on autopsy. However, few cases have been described in non-alcoholic patients, suggesting that alcohol is not the sole responsible for these lesions.
 |
| Marchiafava-Bignami disease |
A, Parasagittal MR T1-weighted image shows multiple areas of decreased signal intensity involving the genu and the anterior aspect of the corpus callosum.
B, MR T2-weighted image corresponding to A shows the lesions to be hyperintense and also some mild atrophy of the involved portions of the corpus callosum.
C, MR Axial T2-weighted image shows a mild degree of periventricular white matter hyperintensity, particularly in the region of the frontal horns of the lateral ventricle.
D, Axial T2-weighted image at the level of the centra semiovale shows a mild degree of periventricular white matter hyperintensities.
📖 Neurology Self-Assessment: A Companion to Bradley’s Neurology in Clinical Practice
Monday, March 22, 2021
Pacini's corpuscles
The structure of the Pacinian corpuscle was described by Pacini (1835). It is widely distributed in mammals and is similar to the Herbst corpuscles found in birds. The Pacinian corpuscle is an ovoid structure about 1 mm in length and is easily seen by the naked eye in a number of locations such as the mesentery.
 |
| Pacini's corpuscles |
On microscopic examination, the lamellar structure of the corpuscle is evident, the lamellae giving an appearance which has been likened to a section through an onion. The corpuscle is innerv!lted by a myelinated sensory axon of medium diameter which terminates within the center of the corpuscle.
Double inferior vena cava
Double inferior vena cava is a vein abnormality that is present from birth (congenital). Individuals with this anomaly have two inferior vena cavas instead of one. The inferior vena cava carries oxygen-poor blood from the lower parts of the body into the heart. Double inferior vena cava does not cause any symptoms. It is usually diagnosed when an imaging test, such as CT or MRI, is performed for other medical reasons. The reported incidence of double inferior vena cava ranges from 0.2 percent to 3 percent
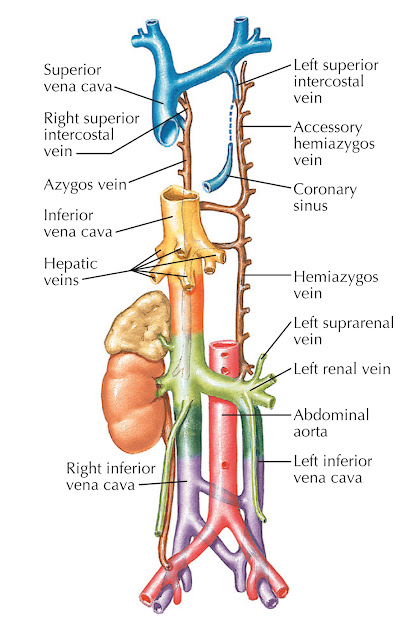 |
| Double inferior vena cava |
A double or duplicated inferior vena cava results from lack of atrophy in part of the left supracardinal vein, resulting in a duplicate structure to the left of the aorta. The common form is a partial paired inferior vena cava that connects the left common iliac and left renal veins. When caval interruption, such as placement of a filter, is planned, these alternate pathways must be considered. As an alternative, the inferior vena cava may not develop. The most common alternate route for blood flow is through the azygous vein, which enlarges to compensate. If a venous stenosis is present at the communication of iliac veins and azygous vein, back pressure can result in insufficiency, stasis, or thrombosis.
Fabry-Anderson disease
 |
| Fabry-Anderson disease |
Saturday, March 20, 2021
Galant's biceps reflex
Biceps reflex is a reflex test that examines the function of the C5 reflex arc and the C6 reflex arc. The test is performed by using a tendon hammer to quickly depress the biceps brachii tendon as it passes through the cubital fossa. Specifically, the test activates the stretch receptors inside the biceps brachii muscle which communicates mainly with the C5 spinal nerve and partially with the C6 spinal nerve to induce a reflex contraction of the biceps muscle and jerk of the forearm.
 |
| Galant's biceps reflex |
A strong contraction indicates a 'brisk' reflex, and a weak or absent reflex is known as 'diminished'. Brisk or absent reflexes are used as clues to the location of neurological disease. Typically brisk reflexes are found in lesions of upper motor neurones, and absent or reduced reflexes are found in lower motor neurone lesions.
A change to the biceps reflex indicates pathology at the level of musculocutaneous nerve, segment C5/6 or at some point above it in the spinal cord or brain.
Left superior vena cava
Left superior vena cava (LSVC) is the most common congenital malformation of the thoracic venous return and is present in 0.3 to 0.5% of individuals in the general population with a normal heart, and 4.5% in individuals with congenital heart diseases. A LSVC co-occurs with the right superior vena cava in 80 to 90% of cases, 2 and may also be accompanied by other heart abnormalities, such as anomalous connections of the pulmonary veins, aortic coarctation, tetralogy of Fallot, transposition of the great vessels as well as dextroversion. Moreover, cardiac rhythm disturbances concerning impulse formation and conduction have been observed.
 |
| Left superior vena cava |
The LSVC
usually drains into the right atrium (in 80–92%) through a dilated coronary
sinus (CS),5,6 but in approximately 10 to 20% of cases, it is associated with
left atrial (LA) drainage. The LSVC may drain directly through the left atrium
or via the unroofed CS, which is a cause of right-to-left cardiac shunt. The
majority of patients with LSVC are asymptomatic. In general, only patients with
unusual drainage and right-to-left shunting are of clinical significance.
Anomalous venous return via the LSVC may be the cause of cardiac arrhythmias,
decreased exercise tolerance, progressive fatigue, chest discomfort,
palpitations, syncope or cyanosis.
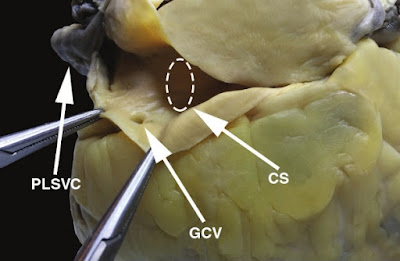 |
| The left superior vena cava drains into the coronary sinus in this heart specimen. CS, coronary sinus; GCV, great cardiac vein; PLSVC, persistent left superior vena cava. |
The implications of existing LSVC could be important for clinicians who are involved in placement of central venous-access devices.
Thursday, March 18, 2021
Galant Reflex
The Spinal Galant Reflex provides the opportunity to experience a change from whole body movements to same side (homolateral) movements. It emerges at 20 weeks in utero, is actively present at birth, and should be integrated by the time the baby is 3 to 9 months of age.
The Spinal Galant Reflex is present when a baby is placed in a prone position (one their stomach) and stimulation is placed to one side of the spine. If the reflex is present, the hip on the side of the stimulus will flex (curl toward that side). This reflex helps the baby to work it’s way down the birth canal during the birthing process, and also allows the fetus to hear and feel the sound vibrations in the womb.
Wednesday, March 17, 2021
Exocrine functions of the pancreas
Each day the pancreas secretes approximately 1 L of alkaline isosmotic pancreatic juice that originates from the pancreatic acinar cells and pancreatic ducts. The colorless, bicarbonate-rich, and protein-rich pancreatic juice plays key roles in duodenal alkalinization and food digestion. The acinar cells secrete the enzymes required for the digestion of the three main food types: amylase for carbohydrate (starch) digestion, proteases (e.g., trypsin) for protein digestion, and lipases for fat digestion. The acinar cells are pyramidal in shape with the apices facing the lumen of the acinus, where the enzyme-containing zymogen granules fuse with the apical cell membrane for release. Acinar cells, unlike the endocrine cells of the pancreas, are not specialized and produce all three types of pancreatic enzymes from the same cell type.
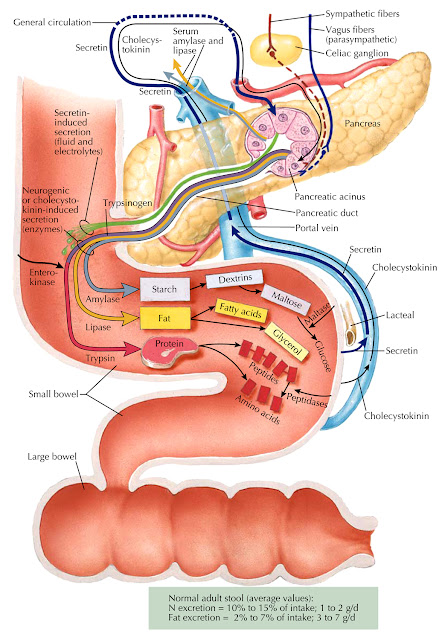 |
| Exocrine functions of the pancreas |
Amylase is secreted in its active form and hydrolyzes starch and glycogen to the simple sugars of dextrins and maltose; maltose is then metabolized to glucose by intestinal maltase.
📖 Transplantation, Bioengineering, and Regeneration of the Endocrine Pancreas: Volume 1
Portal system
The portal system is responsible for transporting blood from most of the gastrointestinal tract to the liver for metabolic processing before the blood returns to the heart. The portal system drains venous blood from the distal end of the esophagus, stomach, small and large intestines, proximal portion of the rectum, pancreas, and spleen. The portal system is the venous counterpart to areas supplied by the celiac trunk and the superior and inferior mesenteric arteries.
 |
| The portal venous system |
The liver is unique in that it receives both nutrient-rich deoxygenated blood (portal vein) and oxygenated blood (hepatic arteries). The portal vein branches as it enters the liver, where its blood percolates around hepatocytes in tiny vascular channels known as sinusoids. Hepatocytes detoxify the blood, metabolize fats, carbohydrates, and drugs, and produce bile. The sinusoids receive deoxygenated blood from the portal veins (provide blood for metabolism and detoxification) and oxygenated blood from the hepatic arteries (provide oxygen for hepatocytes). Blood exits the sinusoids into a central vein, which empties into the hepatic veins and ultimately into the inferior vena cava, which passes through the diaphragm before entering the right atrium of the heart.
 |
| Portal vein. |
Oral drugs travel throughout the gastrointestinal tract, where they are absorbed by the small intestine. These drugs then travel to the liver via the hepatic portal system, where they are metabolized before entering the systemic circulation.
📖 Sleisenger and Fordtran’s Gastrointestinal and Liver Disease- 2 Volume Set
Brachial artery
As a continuation of the axillary artery, it begins at the inferior border of the teres major tendon and it ends at the level of the neck of the radius about 1cm distal to the elbow joint. At this point, it divides into the ulnar and radial arteries. The brachial artery runs medial to the humerus proximally, before moving more anteriorly to lie between the epicondyles of the humerus.
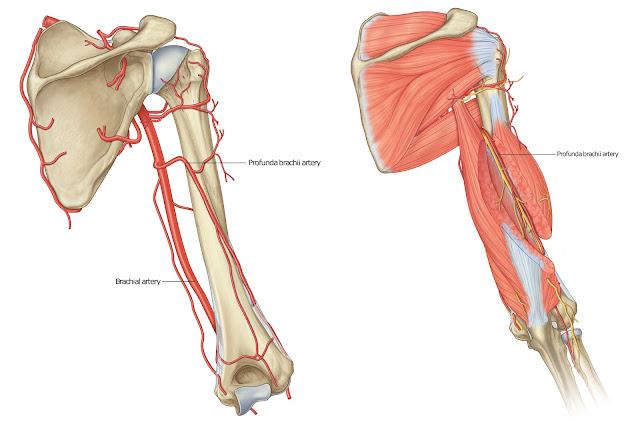 |
| Brachial artery |
Relationships of the brachial artery to other structures in the arm can be important in clinical practice. The brachial artery is a superficial vessel and is only covered by the layers of the skin, as well as the superficial and deep fasciae, with a few exceptions:
The first exception to this is at the cubital fossa, where the bicipital aponeurosis, which is the aponeurosis of the biceps brachii muscle, covers the artery, and separates it from the median cubital vein.
The second exception is when the median nerve crosses the brachial artery near the distal attachment of the coracobrachialis.
 |
| Brachial artery |
Posteriorly, the brachial artery is separated from the long head of the triceps brachii muscle by the profunda brachii artery and the radial nerve. The attachments of the coracobrachialis and the brachialis muscles, as well as the medial head of the triceps brachii muscle, also lie posterior to the brachial artery.
The median nerve and coracobrachialis muscle lie laterally to the brachial artery at its proximal aspect whereas the medial cutaneous nerve of the forearm and the ulnar nerve lie medially to the artery proximally.
Kyphoscoliosis
Kyphoscoliosis has long been recognized as a cause of cardiorespiratory failure. Only in recent years, however, has the combination of clinical picture, physiologic measurements, and anatomic observations at autopsy clarified the natural history of the cardiorespiratory disorder.
 |
| Kyphoscoliosis |
Unless there is independent lung disease, such as bronchitis or emphysema, only patients with severe spinal deformities are candidates for cardiorespiratory failure. Subjects with mild deformities are consistently asymptomatic. In contrast, those with severe degrees of deformity, particularly if considerable dwarfing has occurred, are often restricted in their activities by dyspnea on exertion. They are most prone to cardiorespiratory failure if an upper respiratory infection should supervene. From the point of view of disability and the likelihood of cardiorespiratory failure, the nature of the deformity (i.e., kyphosis, scoliosis, or both) is unimportant when compared with the severity of the deformity and dwarfing.
One approach to classifying individuals with kyphoscoliosis is on the basis of lung volumes. The more normal the total lung capacity, vital capacity, and tidal volume, the more the subject tends to remain asymptomatic. In those with severe reduction in lung volumes, the stage is set for cor pulmonale.
Tuesday, March 16, 2021
Tubuloglomerular feedback
The available evidence suggests that the macula densa, located at the end of the thick ascending limb, senses tubular flow based on the concentrations of sodium and chloride in the local filtrate. The sensing apparatus appears to be apical Na+/K+/2Cl− (NKCC2) cotransporters.
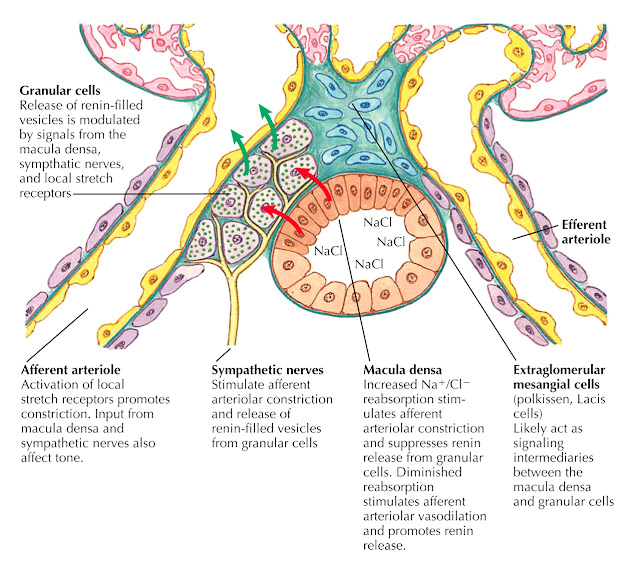 |
| Tubuloglomerular feedback and modulation of renin release |
When tubular fl ow rates are high, there is a slight decrease in solute reabsorption before the macula densa, and thus higher concentrations of sodium and chloride are present at this area. Increased activation of NKCC2 transporters ensues, which leads to constriction of the afferent arteriole and inhibition of renin release.
Cerebral Cortex
The cerebral cortex, a thin layer of gray matter comprising the outer portion of the cerebrum, is the center of the conscious mind. The adult human brain contains almost 98% of all the neuron cell bodies of the nervous system. The cerebral cortex is involved with awareness, communication, sensation, memory, understanding, and the initiation of voluntary movements. Its gray matter contains dendrites, neuron cell bodies, glia, and blood vessels. It lacks fiber tracts but contains six layers in which there are billions of neurons. The cerebral cortex is approximately 2–4 mm thick, yet it makes up approximately 40% of the overall brain mass. Its surface area is nearly tripled by its many convolutions.
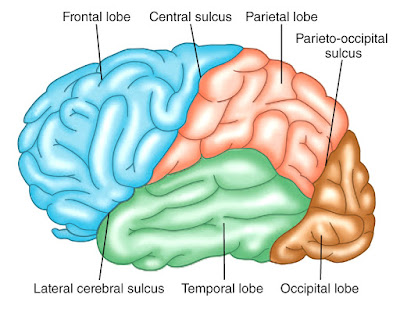 |
| The lobes of the cerebrum. |
Beneath the cerebral cortex is white matter, comprising most of the cerebrum. It contains myelinated axon bundles, some of which pass from one cerebral hemisphere to the other. Others carry impulses from the cortex to nerve centers of the brain and spinal cord.
The lobes of the cerebral cortex are:
■■ Frontal lobe: Forms the anterior portion of each cerebral hemisphere .
■■ Parietal lobe: Lies posteriorly to the frontal lobe.
■■ Temporal lobe: Lies below the frontal and parietal lobes.
■■ Occipital lobe: Forms the posterior part of each cerebral hemisphere.
■■ Insula: Lies under the frontal, parietal, and temporal lobes.
 |
| A coronal section through the cerebrum. The area of gray matter is greatly increased by the folding of the surface into gyri, sulci, fissures, and the insula. |
In most people, one side of their cerebrum acts as the dominant hemisphere, controlling the use and understanding of language. The left side of the cerebrum is usually responsible for activities such as speech, writing, reading, and complex intellectual functions. The nondominant hemisphere controls nonverbal functions and intuitive and emotional thoughts. The dominant hemisphere controls the motor cortex of the nondominant hemisphere.
Eales' disease
Eales Disease is a rare disorder of sight that appears as an inflammation and white haze around the outercoat of the veins in the retina. The disorder is most prevalent among young males and normally affects both eyes. Usually, vision is suddenly blurred because the clear jelly that fills the eyeball behind the lens of the eye seeps out (vitreous hemorrhaging).
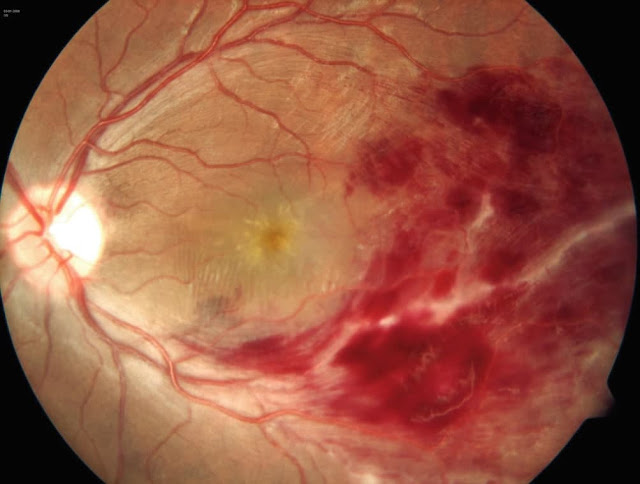 |
| Eales' disease |
Eales Disease usually presents as blurred vision resulting from oozing of the clear jelly-like substance from behind the lens of the eye. At the onset of the disorder, the small outer veins of the retina show sheathing (encapsulation or covering). As the disease progresses, the inflammation around the veins in the retina extends further behind the lens. Eales Disease may also be associated with peripheral retinal neovascularization which is the formation of new blood vessels on the outer part of the retina.
📖 The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology 5th EditionMonday, March 15, 2021
Eagle’s syndrome
Eagle’s syndrome, defined by Eagle in 1949, is characterised by morphological abnormality/ossification of the styloid process. The average length of the styloid process is 20-30 mm in the adult Caucasians and 15.4-18.8 mm in the Asian population. An elongated styloid process is defined by being at least 30 mm long. The clinical picture is composed of recurrent throat and neck pain, radiating into the ear and dysphagia. Symptoms can be bilateral or, more frequently, unilateral. The incidence is 4-8 per 10,000 people.
 |
| Eagle’s syndrome |
The aetiology is not well defined and a number of theories have been suggested, such as congenital elongation due to the persistence of an embryonic cartilaginous outgrowth, calcification of the stylohyoid ligament and formation of bone tissue at the insertion of the ligament. This clinical picture might also be seen in patients after tonsillectomy.
Dabska's tumour
Papillary intralymphatic angioendothelioma (Dabska tumor) is a rarely metastasizing lymphatic vascular neoplasm that usually affects children and young adults. The majority of these cases occur in soft tissues of extremities, and to date less than 40 cases have been described. Despite the generally indolent evolution, can be locally invasive with the potential to metastasize.
 |
| Dabska's tumour - Violaceous lesion, with poorly defined limits, on the sole of the right foot. |
Papillary intralymphatic angioendothelioma (PILA or Dabska tumor) is a rare vascular neoplasm, defined as low grade malignancy tumor, with high tendency of local recurrence.
 |
| Histopathology. Papillary projections with vascular axes lined by rounded and hyperchromatic cells – “Hobnail cells” (Hematoxylin & eosin, ×100). |
Originally considered a malignant tumor and called malignant endovascular papillary hemangioendothelioma, it was renamed in 1998, due to its borderline behavior, prominent presence of lymphatic vessels and the presence of intravascular papillary proliferation.
Caffey-Kempe syndrome
Caffey's landmark article of 1946 noted an association between healing long-bone fractures and chronic subdural hematomas in infancy, and it was the first to draw attention to physical abuse as a unifying etiology. In 1962, Caffey and Kempe et al proposed manhandling and violent shaking as mechanisms of injury and emphasized the acute and long-term sequelae of abuse as serious public health problems. Since these early reports, investigators have more clearly defined the pathophysiology of abusive injuries. Community-service and law-enforcement authorities have taken a role in protecting potential victims and in prosecuting perpetrators.
 |
| Caffey-Kempe syndrome |
In the United States, in 2015, there were 683,000 victims of child abuse, and approximately 1670 children died of abuse and neglect, a rate of 2.25 per 100,000 children. Almost 75% of those deaths occurred in children younger than 3 years. Most reports of abuse were submitted by educational personnel (18.4%) and legal and law enforcement personnel (18.2%). Approximatley 9% of reports were submitted by medical personnel.
For infants and children younger than 2 years, a skeletal survey should be performed as the initial screening examination when child abuse is being considered. The survey consists of the acquisition of a series of images collimated to each body region. The series includes frontal and lateral views of the skull, frontal and lateral views of the spine, frontal views of the chest (ribs) and pelvis, and frontal views of the extremities, including the hands and feet.
Sunday, March 14, 2021
Babington’s disease
Babington’s disease - Osler-Weber-Rendu syndrome (OWR) is also known as hereditary hemorrhagic telangiectasia (HHT). It’s a genetic blood vessel disorder that often leads to excessive bleeding. According to the HHT Foundation International, the syndrome affects about one in 5,000 people. However, many people with the disease don’t know they have it, so this number may actually be higher.
 |
| Babington’s disease |
The name Osler-Weber-Rendu syndrome is named for the doctors who worked on researching this condition in the 1890s. They discovered that issues with blood clotting don’t cause this condition, which was previously assumed. Instead, this condition is caused by problems with the blood vessels themselves.
 | |
| Babington’s disease |
Babcock's operation
The affected veins in the superficial venous system are pulled out through small incisions in the skin (stripped). This procedure is also known as "Babcock's procedure" or "Babcock's stripping". The American doctor Babcock described the method for the first time in 1907. This classic method is used to remove the affected segments of the worst affected long saphenous vein that runs from the ankle up to the inguinal fold.
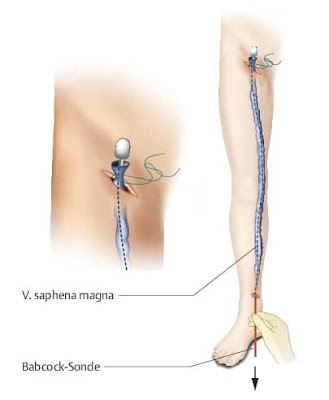 |
| Babcock's operation |
The saphenous vein can only be removed, if the deep venous system is healthy. This is first checked by an ultrasound examination (Doppler ultrasonography), sometimes also with contrast medium X-rays (phlebography). Several days before the procedure, patients should not drink any alcohol or take medicines that delay blood clotting. These include most painkillers.
Friday, March 12, 2021
Pelvic plexus
 |
| Pelvic pleuses |
Calciphylaxis
Calciphylaxis (calcific uremic arteriolopathy) results from deposition of calcium in the tunica media portion of the small vessel walls in association with proliferation of the intimal layer of endothelial cells.
 |
It is almost always associated with end-stage renal disease, especially in patients undergoing chronic dialysis (either peritoneal dialysis or hemodialysis). It has been reported to occur in up to 5% of patients who have been on dialysis for longer than 1 year. Calciphylaxis typically manifests as nonhealing skin ulcers located in adiposerich areas of the trunk and thighs, but the lesions can occur anywhere. They are believed to be caused by an abnormal ratio of calcium and phosphorus, which leads to the abnormal deposition within the tunica media of small blood vessels. This eventually results in thrombosis and ulceration of the overlying skin. Calciphylaxis has a poor prognosis, and there are few well-studied therapies.
Clinical Findings: Calciphylaxis is almost exclusively seen in patients with chronic end-stage renal disease. Most patients have been on one form of dialysis for at least 1 year by the time of presentation.
 |
| Calciphylaxis |
The initial presenting sign is that of a tender, dusky red to purple macule that quickly ulcerates. The ulcerations have a ragged border and a thick black necrotic eschar. The ulcers tend to increase in size, and new areas appear before older ulcers have any opportunity to heal.
Wednesday, March 10, 2021
Dagnini’s reflex
Dagnini’s reflex ( Aschner-Dagnini test, Oculocardiac Reflex)
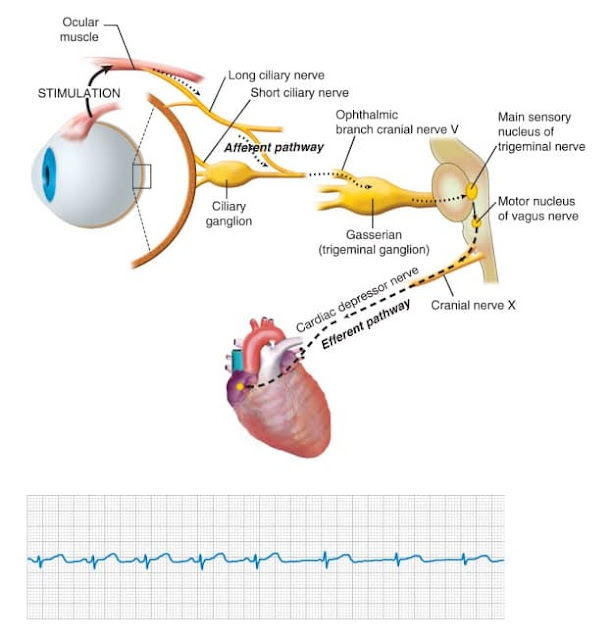 |
| Dagnini’s reflex ( Aschner-Dagnini test, Oculocardiac Reflex ) |
The oculocardiac reflex (OCR), also known as the Aschner reflex or trigeminovagal reflex (TVR), was first described in 1908 as a reduction in heart rate secondary to direct pressure placed on the eyeball. It is defined by a decrease in heart rate by greater than 20% following globe pressure or traction of the extraocular muscles. The reflex most commonly results in sinus bradycardia. However, it also has a reported association with reduced arterial pressure, arrhythmia, asystole, and even cardiac arrest. This reflex has most notably been depicted during ophthalmologic procedures, more specifically during strabismus surgery; however, it also may be activated by facial trauma, regional anesthetic nerve blocks, and mechanical stimulation. This activity describes the oculocardiac reflex and highlights the role of the interprofessional team in the management of patients with the symptoms during surgery.
Anatomy and Physiology
The OCR arc consists of an afferent and efferent limb. The trigeminal nerve, otherwise known as the fifth cranial nerve, serves as the sensory afferent limb.
Baastrup's sign
(Baastrup’s disease, Kissing spines syndrome)
Excessive lordosis is a common finding and may produce mechanical pressure that causes repetitive strains of the interspinous ligament with subsequent degeneration and collapse. Baastrup’s disease (kissing spine syndrome) is a term referring to close approximation of adjacent spinous processes due to degenerative changes of the spine.
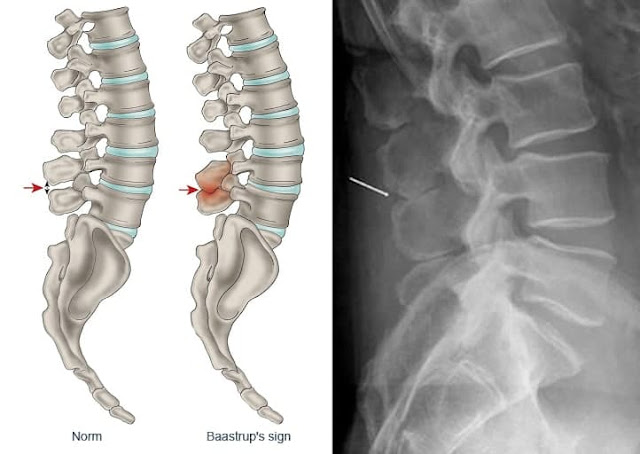 |
| Baastrup’s disease |
Baastrup’s disease usually affects the lumbar spine, with L4-L5 being the most commonly affected level. There is higher occurrence at ages over 70 and no gender predilection. Symptoms include back pain with midline distribution that worsens during extension, is relieved during flexion and is exaggerated upon finger pressure at the level of interest. Diagnosis rests on clinical examination and imaging studies. The hallmark of imaging findings is the close approximation and contact of adjacent spinous processes, with all the subsequent findings including oedema, cystic lesions, sclerosis, flattening and enlargement of the articulating surfaces, bursitis and occasionally epidural cysts or midline epidural fibrotic masses. Proposed therapies include conservative treatment, percutaneous infiltrations or surgical therapies such as excision of the bursa or osteotomy.
Pathogenesis
Baastrup’s disease is a term referring to close approximation of adjacent spinous processes due to general degenerative changes of the spine. Usually there is an excessive lordosis with resultant mechanical pressure process that causes repetitive strains of the interspinous ligament with subsequent degeneration and collapse.
Tuesday, March 9, 2021
Aarskog-Scott syndrome
Epidemiology
AAS prevalence is not known, but less than 100 cases have been reported in the literature since the first description in 1970. However, prevalence estimates are thought to be around 1/25,000. About 40 molecularly proven cases are published worldwide.
 |
| Aarskog-Scott syndrome |
Clinical description
AAS predominantly concerns males. Facial features include widow's peak and hypertelorism, both observed in female carriers, and downslanting palpebral fissures, broad nasal bridge, anteversed nostrils, low set and protuberant ears, maxillary hypoplasia and transverse crease below the lower lip. AAS patients have short and broad hands and feet, interdigital webbing, clinodactyly, and hyperextension of proximal interphalangeal joints and flexion at distal interphalangeal joints causing swan neck deformity of fingers. Size is generally normal at birth, but growth is slow in infancy and childhood, leading to short stature until puberty, which is often delayed. A growth spurt in late teens, generally, results in a moderate short stature. Genital anomalies may include cryptorchidism, macroorchidism, shawl scrotum and, more rarely, hypospadias. Fertility is normal. Female carriers may have only a subtle phenotype with hypertelorism and widow's peak. Patients may present a neurodevelopmental phenotype with learning and behavioural disabilities that are often confined to early childhood. When present, mental impairment is rarely severe.
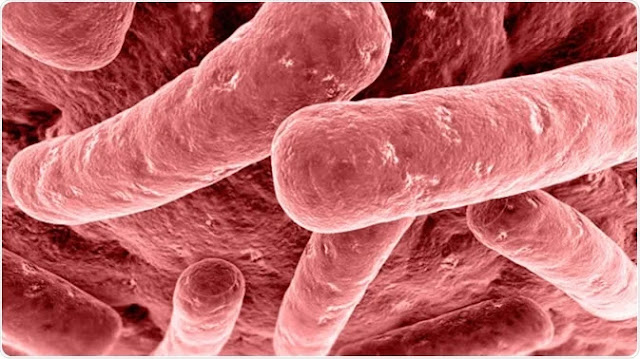
Plague
 |
| Yersinia pestis (Pasteurella pestis) is the bacterium responsible for the bubonic plague. |
 |
Hand of a plague patient displaying acral gangrene. Gangrene is one of the manifestations of plague and the origin of the term Black Death given to plague throughout the ages. |
Sunday, March 7, 2021
Adamson's fringe
Adamson's fringe is located at the upper margin of the keratogenous zone of the hair follicle where the nucleated hair shaft cornifies completely and gets converted to hard anucleated keratin.
 |
| Adamson's fringe |
It marks also the area of complete keratinization of the cuticle and Henle's layer of the inner root sheath and the beginning of the stem of the follicle. In Tinea capitis, dermatophytic infection of the hair shaft is restricted to this zone and the fungi do not penetrate further down the infected hair in the bulb of the follicle. The fungi in Adamson's words form “a fringe of mycelium surrounding the hair shaft and project below the lower margin of the sheath of spores around the root-stem.”
The keratogenous zone of the hair follicle is a broad area above the bulb of the follicle in which the cells are gradually transformed into hard keratin of the hair shaft.
Friday, March 5, 2021
Botulism
Botulism is a rare but fatal disease caused by botulinum toxins released from Clostridium botulinum bacteria. Botulism is categorized into five different forms: foodborne botulism, wound botulism, infant botulism, inhalation botulism, and iatrogenic botulism.
 |
| Botulism is a potentially fatal condition that is caused by a bacterium called Clostridium botulinum. |
Agent: Botulinum toxin, produced by the anerobic sporeforming bacterium Clostridium botulinum types A, B, E and rarely F. Type E and F neurotoxins have been recovered from infants with botulism due to C. butyricum and C. barati. C. botulinum is considered a biological warfare agent.
Reservoir: C. botulinum spores are found in soil, dust, honey, marine sediments, and in intestines of fish and land animals.
Transmission: By ingestion of contaminated food (honey in infant botulism), injection of contaminated drugs, or contamination of wounds by soil, dust or gravel. There is no human-to-human transmission.
 |
| Clostridium botulinum gram stain. |
Incubation period: Usually 12–36 hours; sometimes several days; up to 2 weeks for wound botulism. Clinical findings: Descending flaccid skeletal muscle paralysis beginning at the shoulders in the absence of fever; fatigue, weakness, vertigo, blurred vision, dry mouth, difficulty in speaking and swallowing, progressing to an inability to breathe without assistance. Vomiting, diarrhea or constipation may occur. The CFR in the USA after treatment is 5–10%; recovery may take months. Infants present with constipation, anorexia, weakness, an altered cry, difficulty sucking, and swallowing. Muscle weakness progresses in a symmetric descending fashion over hours to a few days. The prognosis is excellent when treated timely.
Wednesday, March 3, 2021
Renin–angiotensin–aldosterone system (RAAS)
The Renin-Angiotensin-Aldosterone System (RAAS) is a hormone system within the body that is essential for the regulation of blood pressure and fluid balance. The system is mainly comprised of the three hormones renin, angiotensin II and aldosterone. Primarily it is regulated by the rate of renal blood flow.
 |
| The renin–angiotensin–aldosterone system (RAAS). |



